Nurturing Well-Being
Second Opinion
How can the health-care workforce recover from pandemic burnout?
In many ways, the well-being of our clinical care teams drives the quality of care we deliver and our rate of medical error. But well-being can suffer when a health-care provider experiences burnout, a phenomenon that occurs when providers reach a point where they have given more of themselves than is healthy. Symptoms include exhaustion, mental distance from one’s work and a sense of lacking efficacy in the job.
Burnout is a concept originally described for the “giving” professions, especially those that are mission-driven, where employees expect themselves and others to go above and beyond. In the health-care field, our training focuses on what’s best for the patient, not what’s best for individual doctors and nurses. As high achievers, many of us enter health care believing we can solve any problem if we only try hard enough. We are applauded for always going the extra mile and can develop a superhero mentality that makes it difficult to ask for help.
A national survey published annually by Medscape reveals that 79 percent of physicians reported that their burnout started before the pandemic. So, burnout is not something that happened just because of the pandemic. In fact, at Weill Cornell Medicine, we didn’t see burnout skyrocket and well-being plummet during the peak of the pandemic, despite the intensity and stress of our work during that time. Why?
The pandemic gave many clinicians a profound sense of meaning and belonging to a community, which research shows can play a protective role and inoculate people, to some extent, from burnout. But we do have data indicating that the incidence of post-traumatic stress disorder, anxiety and depression during the pandemic increased not only in the general population but also among health-care providers. Addressing that, and addressing burnout, involve destigmatizing and normalizing mental health care, while embracing the idea that just as everyone needs a primary care physician, perhaps everyone — health-care workers included — needs a mental health care provider.
In typical academic medical centers, burnout rates hover at around 40 percent. Our rates are slightly lower at Weill Cornell Medicine, but we still have a lot of work to do to make sure our clinical care teams feel valued, receive appropriate feedback and support from supervisors, have the opportunity to experience ownership and growth in their jobs, and have resources available to lessen the burden of electronic health records. More than anything, our surveys tell us that our physicians want to be part of strong, high-performing teams. Nurses have been earlier to recognize that a “go it alone” mentality is unsustainable. Physicians, due to traditional medical training that encourages individual achievement, have more room to grow in this area.
“Burnout occurs when providers reach a point where they have given more of themselves than is healthy. Symptoms include exhaustion, mental distance from one’s work and a sense of lacking efficacy in the job.”
Humans don’t like uncertainty, and we went through more than two years of extraordinarily uncertain times during the pandemic. We all have developed a variety of tools to cope with the stressors of daily life, such as sticking to certain routines. The pandemic depleted those toolkits, potentially requiring us to resort to tools we’ve never used before — or to suffer the consequences.
Some of Weill Cornell Medicine’s own researchers, including Dr. Benjamin Zebley, an assistant professor of psychiatry, and Dr. Conor Liston, an associate professor of neuroscience and psychiatry, conducted what is probably the largest naturalistic study of stress among U.S. health-care workers throughout the pandemic. For this, they tracked longitudinally symptoms of anxiety, stress, depression, sleep issues and social isolation among NewYork-Presbyterian employees, discovering, not surprisingly, that signs of distress kept going up throughout the pandemic, almost in a cumulative way. But the big takeaway from the study — the real punchline — is this: more than any other factor, social isolation put our health-care workers at risk of significant anxiety and depressive symptoms.
This finding aligns with another major study published recently by researchers at the University of Michigan, looking at mental health symptoms of first-year training physicians (interns) nationwide. This one, too, identified social isolation as the biggest risk factor for anxiety and depression. What, then, can these studies tell us?
They tell us that the best hedges against stress, anxiety and depression are to decrease isolation and instill social support among our staff. They suggest, too, that a key component to wellness involves a feeling of “belonging” to a team and that you are part of something bigger than yourself. Wellness is not a single-dose treatment, but requires an attitudinal shift to conceptualize it as something to work at and surveil continuously, as part of our daily life. Just as we need to exercise daily, we need to incorporate routines such as mindfulness and mental health checks.
For health-care workers, some degree of stress will always exist because of the nature of our jobs. That’s why we’re continuing to offer CopeNYP, the free, emotional well-being resource and counseling service launched during the pandemic and used by more than 7,000 NYP employees. During the pandemic, we had to do things reactively, but moving forward, we must do things proactively to enhance our own wellness and resilience.
Emergency physicians and, really, all health-care providers were already experiencing increased burnout, even before the pandemic hit. Then suddenly, we were confronted with an unprecedented health crisis — one that pushed our hospital resources to a breaking point.
As emergency clinicians, we’re always available and on the front line. This unique role was challenging during the height of the pandemic because we not only treated emergency room patients but also served as the safety net for all patients, given that medical and primary care practices were largely unavailable. As providers, we were keenly aware of the inherent risks we undertook and posed to our loved ones — a reality compounded by seeing our colleagues grow ill or even succumb to the virus. It was a tough time.
Several years before the pandemic, we had established a wellness and peer support program to combat rising burnout. Our nationally recognized program centers around peer support, which is a critical component, given that our peers can simultaneously offer a different perspective and understand what we’re feeling. We implemented a three-pronged peer support program for faculty that involved group discussions about wellness-related topics; one-on-one peer support for any staff member experiencing a patient death or bad outcome; and social outings outside of the hospital.
In the clinical environment, it’s important to create calm spaces and institute formal breaks from clinical work to allow for protected time to relax or eat a snack or meal. We redesigned our faculty offices and common areas with this in mind. Likewise, it’s especially critical to alleviate administrative tasks. We live in a culture of information overload, where health-care providers receive a high volume of messages, alerts and texts that can take us away from patient care. Although electronic health records connect patients with clinicians, we need to be mindful of “alert fatigue” by monitoring the well-being of our clinical staff on the receiving end of messages and texts. We also need to make documentation easier, which may include virtual scribes, a dictation software or some other technological solution.
Without question, one cannot effectively take care of others if one cannot take care of oneself. We must support and meet the needs of our frontline staff, so they can provide high-quality care for our patients. A robust wellness program, such as the one we’ve created in our department and continue to build, facilitates exactly that.
Portraits: Rebecca Clarke
Summer 2023 Front to Back
-
From the Dean

Message from the Dean
As Weill Cornell Medicine marks the 125th year since its founding, it is striking to reflect upon how our values have endured. -
Features
Window Into the Future
An ambitious research program could hold clues to improving the health of women and their children across their lifespans. -
Features
Caught on Camera
Recordings made in Dr. Simon Scheuring’s lab reveal how elusive molecules embedded in cell membranes get their jobs done — for good and ill. -
Features

Risks and Rewards
Alumnus Dr. Anthony Fauci (M.D. ’66) joins Dr. Jay Varma in a candid conversation about the future of public health and more. -
Notable

Two Landmark Anniversaries
Weill Cornell Medicine is celebrating more than a century of excellence in medical education, scientific discovery and patient care, commemorating 125 years since its founding. -
Notable

Honoring Diversity
In a celebration of Weill Cornell Medicine’s commitment to fostering diversity, equity and inclusion in academic medicine, the institution honored nearly a dozen faculty, students and staff. -
Notable

Overheard
Weill Cornell Medicine faculty members are leading the conversation about important health issues across the country and around the world. -
Notable

News Briefs
Notable faculty appointments, honors, awards and more — from around campus and beyond. -
Notable

Dateline
The Salzburg-Cornell Seminars, now part of the Open Medical Institute (OMI), celebrates 30 years of knowledge-sharing, having served more than 26,000 fellows from 130 countries. -
Grand Rounds

There Is Hope
How immunotherapy offered a new lease on life -
Grand Rounds

Medical School, Minus the Debt
Weill Cornell Medicine’s debt-reduction program. -
Grand Rounds

News Briefs
The latest on teaching, learning and patient-centered care. -
Discovery
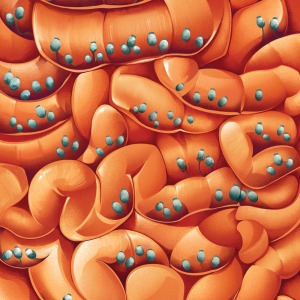
Filling a Critical Gap in the Gut
An important discovery positions fungi as a missing part of research on how the gut biome influences health. -
Discovery

New Clues to Coma Recovery
Delays in regaining consciousness may serve a purpose: protecting the brain from oxygen deprivation. -
Discovery

Findings
The latest advances in faculty research, published in the world’s leading journals. -
Alumni

Profiles
Forging critical connections to move research from the bench to the bedside, our alumni are making an impact. -
Alumni

Notes
What’s new with you? Keep your classmates up to date on all your latest achievements with an Alumni Note. -
Alumni
In Memoriam
Marking the passing of our faculty and alumni. -
Alumni

Moments
Marking celebratory events in the lives of our students, including Match Day and Graduation. -
Second Opinion

Nurturing Well-Being
How can the health-care workforce recover from pandemic burnout? -
Exchange

High-Risk, High-Reward
Two enterprising scientists discuss how the ecosystem for innovation at Weill Cornell Medicine provides the support entrepreneurial faculty and students need to turn their promising research into commercially viable drugs and other treatments. -
Muse

In the Flow
Dr. Navarro Millán is a rheumatologist, clinical investigator and multi-instrumentalist. -
Spotlight

Making Health Care Affordable and Equitable
Dr. Cheryl Pegus (M.D. ’88) is a cardiologist working in health-care businesses on new products to meet consumer needs, enhance health equity and improve health outcomes.


