I don’t think that mandates should be the rule. I don’t think that constraining people should be the rule. But sometimes you temporarily have to get people to do things that they may not fully agree with for the better of society.
Dr. Varma: Individuals can find ways to convince people in their immediate circle, but the challenge really ends up being one for government. Are there lessons from COVID about how you can get governments to view this threat as real and take actions to mitigate that type of threat?
Dr. Fauci: Pandemics are an evolving and phased situation because you don’t face a full-blown pandemic on Day One, and that’s one of the things we faced in a very problematic way with COVID. We’ve got to learn to reach out better and get the community involved in understanding the complexity of the decision-making process because it isn’t simple when you’re dealing with a dynamic process, in essence a moving target.
Dr. Varma: You need to have a baseline infrastructure that can manage all threats. What is the public health infrastructure you think that the U.S. needs that it doesn’t have right now?
Dr. Fauci: We have got to rebuild our local public health infrastructure, which failed us somewhat. The positive lesson is in the realm of science, where the investment over decades in basic and clinical biomedical research was responsible for our ability to go from a [SARS-CoV-2] sequence on January 10, 2020, and 11 months later, a vaccine. That is beyond unprecedented in the annals of vaccinology.
Dr. Varma: I want to go back and understand your training at what is now Weill Cornell Medicine and New York-Presbyterian/Weill Cornell Medical Center. How did all of that come together to shape your professional aspirations, particularly as a physician-scientist?
Dr. Fauci: When I went to Weill Cornell Medicine, the one thing I wanted to do was be a clinically practicing doc. I had no desire to get involved in research, certainly not fundamental basic research.
But then I took a fellowship in infectious diseases/immunology at the NIH. And even though I was 100% convinced that I wanted to come back and practice with my heroes — all the Rees Pritchetts, the Aaron Feders, Elliot Hochsteins and the Jerry Barondesses, among others — I found out there was something else that I liked and I was good at, and that was research.
I stayed at the NIH for three years, and I wasn’t quite sure what I wanted to do. I came back to be chief resident in 1971-72. It was one of the most enjoyable years of my life, but I became convinced halfway through that I could do basic and clinical research and still see patients, and so I returned to the NIH, where I remained for half a century.
Dr. Varma: How did your role evolve to being one where you were at a much higher level of shaping public policy?
Dr. Fauci: The thing that changed it all for me was HIV. It was very, very clear that the attention that was being paid by the federal government was not up to the level it deserved. And the only way that I saw that I could change that was to do something that I did reluctantly, but then with a lot of encouragement from my mentors. I decided I was going to accept this position as the director of NIAID and learn what it was like to get involved in policy and going beyond your own field.
It became clear to me that the activists were correct: We were being too rigid from a regulatory and a scientific standpoint about how we were addressing a very unique situation. I learned what it meant to really push for a concept that might break some of the established paradigms, and the more I got into it, all of a sudden there were other things that needed that type of approach. There was malaria and there was tuberculosis. There was pandemic influenza. And then we had Ebola and Zika.
You find out that if you can present the scientific facts and evidence to people in high levels of policy, that you can get things done that you’re never able to get done in your lab or your clinic.

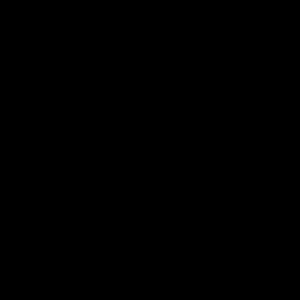
Dr. Anthony Fauci (M.D. ’66), left, with Dr. Jay Varma in a photo composite.
Dr. Varma: There’s a real urgency to restore faith in public health, and activists can play a major role in that. I’m wondering whether all of that advocacy that played such an important role in shaping HIV policy can be leveraged to what we’re doing now in dealing with COVID, both in improving public health practice, and also advocating for and improving the science.
Dr. Fauci: It’s a different situation. When we were dealing with the AIDS activists, we were dealing with a group who had a very, very important message that was value added, and it was up to us to realize that fact. We were able to become partners in our common goal of what we needed to accomplish. It was a reaching out and listening to other people.
Today with COVID, I think it’s much more complicated because we have divisiveness that even goes beyond normal politics. But we should not give up in reaching out, even if certain elements in the community are acting in a way that looks like they’re attacking you and are really dead set against anything you’re trying to do with regard to getting people vaccinated, getting people boosted, doing the kinds of mitigation that are important to control an outbreak.
Dr. Varma: One of your intentions is, in this very active retirement, to encourage physicians and scientists to participate in public service. What should they do to prepare themselves?
Dr. Fauci: There are many, many pathways to a career in public health. You could go the physician training. You could do the epidemiology training. You could do a master’s and then a Ph.D. in public health. The end game is the same: You want to improve the public health of your country and the world.
Dr. Varma: I think one of the challenges, once you finally arrive in that leadership role, is that a lot of people with a medical or scientific background don’t get a lot of training in how to make and communicate high-consequence policy decisions, [and in] how you navigate these complex leadership and organizational structures. How do you think they can start to practice or learn some of these skills before they get to that role?
Dr. Fauci: You get yourself hooked up with a mentoring situation. It could be with someone who’s a public health leader. You could do it by even taking an internship in politics, or go to an organization. There are so many different pathways.
Dr. Varma: Another challenge, of course, is that when you move into these policy roles, it depends on the input of the public. You can’t simply take the information that’s in medical science and immediately translate it. We now face a world in which what we thought was a common set of facts — and we may have different policy recommendations based on that — has now changed. People are really disputing that common set of facts and with a velocity and intensity that I don’t think we’ve seen before. I’m curious about how you view this threat of misinformation [in which] the facts themselves are often in dispute.