
Scientists Target Human Stomach Cells for Diabetes Therapy
Discovery

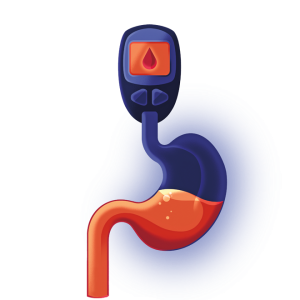
Stem cells from the human stomach can be converted into cells that secrete insulin in response to rising blood sugar levels, offering a promising approach to treating diabetes, according to a preclinical study from researchers at Weill Cornell Medicine.
In the study, published in Nature Cell Biology, researchers at the Hartman Institute for Therapeutic Organ Regeneration showed that they could take stem cells obtained from human stomach tissue and reprogram them directly into cells that closely resemble pancreatic insulin-secreting beta cells. Transplants of small groups of these cells reversed signs of disease in a mouse model of diabetes.
“This is a proof of concept study that gives us a solid foundation for developing a treatment, based on patients’ own cells, for type 1 and severe type 2 diabetes,” said senior author Dr. Joe Zhou, who has been working on cell-based solutions for diabetes therapy for more than 15 years.
An estimated 1.6 million Americans have type 1 diabetes, which results from an autoimmune attack that destroys beta cells in the pancreas. An additional several million have severe type 2 diabetes.
Biomedical researchers aim to replace beta cell function in a more natural way, with transplants of human cells that work like beta cells: automatically sensing blood sugar levels and secreting insulin as needed. Ideally, transplants would use patients’ own cells to avoid the problem of transplant rejection.
In this new study, led by first author Dr. Xiaofeng Huang, researchers discovered that human gastric cells could be turned into insulin-producing beta cells by forcing the activation of three transcription factors or proteins that control gene expression, resulting in the subsequent activation of genes required for the development of normal beta cells.
When the team grew the cells in small clusters called organoids, they found that these organ-like pieces of tissue quickly became sensitive to glucose, responding with secretions of insulin. When transplanted into diabetic mice, the beta-like organoids suggested good durability and functioned largely as real pancreatic beta cells would, secreting insulin in response to rises in blood glucose, thereby keeping blood glucose levels steady.
Dr. Zhou said that he and his lab still need to optimize their method in various ways before it can be considered for clinical use.
Ultimately, the researchers hope to develop a technique enabling the relatively easy harvesting of gastric stem cells from patients, followed by the transplant of insulin-secreting organoids that regulate blood sugar levels without the need for further medication.
Illustration: Ollie Hirst
Fall 2023 Front to Back
-
From the Dean

Message from the Dean
New Dean Robert A. Harrington, M.D. reflects on Weill Cornell Medicine’s tripartite mission — to care, to discover and teach — and ways to deepen and advance these goals. -
Features

Cancer Vaccines’ Promise
Patients are closer than ever to benefiting from a new treatment approach, thanks to strides in immunotherapy and COVID-19 vaccine technology.
-
Features

Silent Partners
How the brain’s less celebrated cells may drive Alzheimer’s disease and other dementias. -
Features

Future Forward
Dean Robert A. Harrington, M.D., shares his vision for Weill Cornell Medicine in a wide-ranging Q&A.
-
Notable

A New Residence for Graduate and Medical Students
A modern new residence on the Upper East Side campus will enhance the student experience. -
Notable
Dateline
Dr. Jyoti Mathad’s research could transform maternal health in under-resourced countries. -
Notable
Overheard
Weill Cornell Medicine faculty members are leading the conversation about important health issues across the country and around the world. -
Notable

News Briefs
Notable faculty appointments, honors, awards and more — from around campus and beyond. -
Grand Rounds

Playing With Heart
A transplant serves up a new beginning. -
Grand Rounds

An End to Suffering in Silence
Weill Cornell Medicine’s Center for Female Pelvic Health is committed to treating women with dignity. -
Grand Rounds
News Briefs
The latest on teaching, learning and patient-centered care. -
Grand Rounds
3 Questions
During the COVID-19 pandemic, Weill Cornell Medicine adapted medical education. It wasn’t the first time the institution responded to historic public health events. -
Discovery
Making a Male “Pill”
A new “on-demand” method in development could offer men another choice for contraception. -
Discovery
Scientists Target Human Stomach Cells for Diabetes Therapy
Stem cells from the human stomach offer a promising approach to treating diabetes.
-
Discovery

Findings
The latest advances in faculty research, published in the world’s leading journals. -
Discovery
3 Questions
Dr. Gunisha Kaur and the team at the Weill Cornell Medicine Human Rights Impact Lab are finding ways to improve refugee health. -
Alumni

Profiles
From serving vulnerable communities to forging critical connections to move research from the bench to the bedside, our alumni are making an impact. -
Alumni

Notes
What’s new with you? Keep your classmates up to date on all your latest achievements with an Alumni Note. -
Alumni
In Memoriam
Marking the passing of our faculty and alumni. -
Alumni

Moments
Marking celebratory events in the lives of our students, including the White Coat Ceremony and receptions for new students. -
Second Opinion
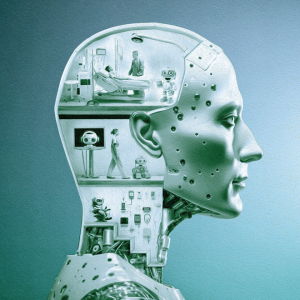
AI in RX
How can chatbots be used in medicine? -
Exchange

Diversifying Medicine
Two physicians discuss the unique experiences of Latino men in medicine and the crucial need for diversity. -
Muse

Writing to Make Meaning
Dr. Rachel Kowalsky is a pediatric emergency physician and an award-winning author. -
Spotlight

At the Forefront of Immunometabolism
Dr. Ke “Dave” Xu (Ph.D. ’21) and Dr. Anjin Xianyu (Ph.D. ’20), the founders of META Pharmaceuticals, are developing treatments for autoimmune diseases.