Hungry for More Choices
Historically, efforts to prevent pregnancy have centered on women because they have the sole ability to become pregnant. But men have long sought a role in family planning, Dr. Levin explains. Condoms came into use around 2,000 years ago. Doctors performed the first human vasectomy in 1899. Unfortunately, these two options — the only forms of male birth control currently available — are unacceptable for many men, which has helped to drive up the global birth rate. Today, half of all pregnancies are unintended, according to the United Nations Population Fund.
Although researchers have been working on new options for men since hormonal birth control for women came to the U.S. market in the 1960s, efforts toward making new male contraceptives have largely hit dead ends, says Dr. Logan Nickels, research director at Male Contraceptive Initiative (MCI), an organization that provides funding and advocacy support for male contraception research and development, including for the LevBuck Lab.
“The joke in the field is that we’ve been 10 years away from a new method for male contraception for the past 50 years,” he says.
Hormonal methods geared toward preventing sperm production — the mainstay of male contraception research — have demonstrated significant promise, said Dr. Nickels. However, in clinical trials, they have also shown many of the same side effects as hormonal contraceptives for women: acne, mood swings and weight gain. These methods also take months to build efficacy in individuals, and months more for individuals to regain their fertility once their use ends. Because men don’t have the same medical risks that accompany contraception failure in women (pregnancy and childbirth are fatal for nearly 300,000 women worldwide annually, according to the World Health Organization), investigators believe the side effects and health risks for a male contraceptive must be much lower than those for females to gain regulatory approval.
Men are hungry for more choices, explains Steve Kretschmer, founder and executive director of the consultancy firm DesireLine, which in 2002 surveyed over 18,000 men in the United States and in six low- and middle-income countries for the Bill and Melinda Gates Foundation and MCI to help the foundations make decisions around investments and impact in family planning. In April of 2022, some 39% of U.S. men surveyed reported intent to use new male contraceptives within 12 months of availability. In May of 2023, this intent rose to 49% after the Supreme Court’s Dobbs v. Jackson decision that revoked the constitutional right to abortion.
A “Sticky” Challenge
The LevBuck’s lab research in male contraception started in the late 1990s, after Dr. Levin and Dr. Buck joined Weill Cornell Medicine, shared lab space and became friends.
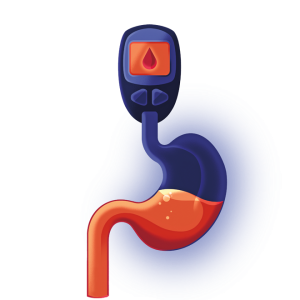
In 1999, the two scientists identified sAC after searching for molecules that produced cAMP, a messenger molecule that plays numerous roles in the body and was the focus of Dr. Levin’s lab. Energized by their discovery, the researchers combined their labs to jointly study this new molecule. Using preclinical models, they soon discovered that sAC was necessary for sperm motility upon ejaculation, a finding that immediately drew the attention of pharmaceutical companies interested in developing a male contraceptive. But these hopes were dashed when the LevBuck lab found that sAC is produced throughout the body, not just in sperm — if men took drugs to block sAC’s action in sperm, it could potentially affect numerous systems in the body, leading to unacceptable or potentially dangerous side effects.
“This killed the project,” Dr. Buck says. But the project found new life after Dr. Balbach’s discovery in 2019. After her momentous presentation at the lab meeting, Drs. Levin and Buck immediately called their colleague Dr. Peter T. Meinke at the Sanders Tri-Institutional Therapeutics Discovery Institute (TDI), a nonprofit established to help promising academic discoveries at Weill Cornell Medicine, The Rockefeller University and Memorial Sloan Kettering Cancer Center move from scientific labs to patients.
Dr. Meinke, the Sanders Director at the TDI, and his colleagues there were already working with the LevBuck lab, using medicinal chemistry to bring a rudimentary sAC inhibitor they had developed into a compound that pharmaceutical companies might be interested in licensing as an ocular hypotony treatment. But while eye drops are delivered to a somewhat restricted space, limiting potential safety concerns, a male birth control pill would be systemic, significantly raising the chance of effects that could impact other parts of the body. As an additional challenge, a male pill focused on sAC would also need to be “sticky,” adhering to its target (the sperm) for hours even after sperm exited the male body and entered the female one (if the drug doesn’t stick long enough to sAC in females, sperm motility could resume, resulting in pregnancy).
New research published by another lab a couple weeks after Dr. Balbach’s presentation reassured the researchers that a systemic sAC inhibitor would have little risk, especially if only taken temporarily. This study showed that two Iranian farmers who both had mutations that shut off their sAC genes had few health issues other than being completely infertile. The second requirement of developing a very “sticky” molecule would prove trickier.
“Imagine that each sperm is a car that needs a key to start,” Dr. Meinke explains. “We’re trying to design a toothpick that fits perfectly in the ignition and can keep it blocked for hours, so the key doesn’t fit.”
In February 2023, the team published a proof of concept study in male mice using a compound called TDI-11861. When the researchers injected this compound into the animals, their sperm remained immotile for about 2.5 hours. Although these animals displayed normal mating behaviors, the treated mice produced no pregnancies if they mated during this time period. Some breakthrough pregnancies occurred with matings beyond this limit, and fertility for all the animals returned to normal by the next day.
Based on the enormous interest this research generated, Drs. Buck and Levin, along with Dr. Meinke and other colleagues, started a new pharmaceutical company called Sacyl Pharmaceuticals to continue developing a sAC-inhibiting male contraceptive, and in August, the LevBuck lab received a $6 million NIH grant to further develop clinical lead compounds and test the concept in a second, preclinical animal model. (Weill Cornell Medicine Enterprise Innovation, which accelerates the translation and commercialization of technologies arising from research conducted by Weill Cornell faculty and trainees, is leading the out-licensing of the team’s discovery to their start-up company; the lab’s federal funding does not support Sacyl Pharmaceuticals’ activities.) Although there are many challenges ahead in developing a compound that men can take orally, stays stable in the body and remains adhered to its target — factors all being addressed in ongoing medicinal chemistry work — Dr. Balbach, now an assistant professor at Michigan State University, believes it’s not only possible, but that having this new option could revolutionize cultural thinking around men’s role in family planning.
“Even if our drug should fail for some reason, I think we’ve already done something great,” she says. “We have opened people’s minds to new possibilities.”
Drs. Levin, Buck and Meinke are equity stakeholders in Sacyl Pharmaceuticals and inventors on a patent licensed to the company.