Image Making
Second Opinion
How will today’s advances in radiology transform patient care?

Dr. Robert J. Min, M.D. ’90
Professor and Chair of Radiology
John A. Evans, M.D. Professor of Radiology
President & CEO, Weill Cornell Physician Organization
Radiologist-in-Chief, NewYork-Presbyterian / Weill Cornell Medical Center
President, Weill Cornell Imaging at NewYork-Presbyterian
As chair of radiology, I see a bright future. I predict that in 10-20 years, the data-rich medical specialties — imaging, pathology, genomics — will become a new specialty called diagnostic and predictive medicine. Technology will allow such specialists to do much more, to truly transform care and save lives through early detection and prevention. Increasingly, these “information specialists” will be the ones communicating with patients and playing a bigger role in managing diseases — even determining next steps.
Advances in medical imaging can help us deliver improved multidisciplinary care. For example, patient compliance on statins and other medications is often not great. Detailed pictures of a patient’s diseased arteries combined with AI-driven predictions of their specific risk for significant cardiac events could drive compliance and dramatically improve patient care.
Weill Cornell Medicine has many tools and technologies to transform health care. We are one of the first medical centers in New York with a 7-Tesla MRI, which offers far more detail than a traditional MRI. Ours is unique because we hope to use it for clinical research — its traditional use — and clinical care to take full advantage of novel therapies. With patients who have epilepsy, for example, we can identify the specific focal area in the brain responsible for the seizure activity, giving clinicians more anatomic detail to determine a better, more targeted treatment plan.
Our new photon-counting CT Scan will offer unbelievable advances in spatial resolution, particularly for heart patients. In the past, interventional radiologists like myself had to inject dye directly into the blood vessel to visualize it. In more recent years, CT angiography of the heart allowed us to see narrowings of the blood vessel but until photon-counting CT, the spatial resolution was not quite good enough to provide the level of detail needed to make accurate predictions. For the first time, we can now look at atherosclerotic plaque that narrows blood vessels and characterize it as chronic, heavily calcified versus fatty, vulnerable plaque that is more prone to causing a heart attack. These new insights into an individual’s risk for a significant cardiac event have implications on how to treat patients through interventions or with medications.
We are also making advances in breast imaging and dedicating space to provide perhaps the most comprehensive women’s imaging program in the country. Breast MRI has a much higher sensitivity for detecting breast cancers in women with dense breasts — which affects 50% of women over 40 — than mammography or ultrasound, but it is currently more expensive. Advances in AI allow us to now perform follow-up breast MRIs in much less time, in most cases as fast as seven minutes. Ultimately, faster exams result in decreased cost, making this technology far more affordable for many more women.
Ultimately, we hope to integrate advanced imaging, AI, genomics and liquid biopsy at our new clinical facility at 575 Lexington Ave. We believe this will improve early detection of disease, enhance patient outcomes and reduce long-term health-care costs.

Dr. Mert R. Sabuncu
Professor of Electrical and Computer Engineering, Cornell Tech and Meinig School of Biomedical Engineering
Vice Chair of AI and Engineering Research, Department of Radiology, Weill Cornell Medicine
AI will transform radiology and diagnostic medicine in the next five years. A radiologist reads a scan for anatomical, physiological indications that might correlate with symptoms, but few quantitative measurements are extracted because it’s laborious, time-consuming, prone to error and hard to standardize. There’s a real opportunity for AI to develop algorithms to extract rich, quantitative information from images through faster, more affordable and less invasive tests. For example, with CT scans and AI, we can reduce the X-ray dosage significantly and get similar quality images, exposing the patient to less radiation.
In the context of AI-enhanced imaging, Dr. Martin Prince and I are studying patients with progressive polycystic kidney disease who get annual abdominal MRIs. Their cysts proliferate and grow, and we need to keep track of the number, size and type of cysts, how they impact organs and overall abdominal health. Today, the standard of care in radiology does not entail a detailed quantitative characterization of these aspects, in part due to time constraints. An AI system that we are building, on the other hand, allows us to compute the size and the numbers of cysts and the volumes of organs to a very high precision and with minimal human effort in a time-efficient way. We believe this technology can be transformative in extracting rich quantitative information from clinical scans that will be critical for the clinical management of patients.
In another collaboration with cardiologists, we are exploring AI’s role in opportunistic screening. Chest CT scans are typically performed for lung cancer screening or lung health assessment, but these images capture far more than just the lungs. In collaboration with Dr. Nir Uriel and Dr. Ashley Beecy, we are investigating how AI can leverage large-scale imaging data to detect early signs of conditions such as heart failure. This could enable the identification of asymptomatic patients, allowing them to receive advanced therapies before symptoms develop.

Dr. Gloria Chiang
Professor of Radiology
Vice Chair of Clinical and Translational Research, Department of Radiology
Director, Brain Health Imaging Institute
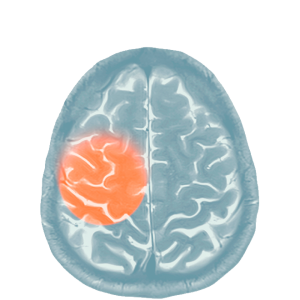
In the last decade, radiology, especially neuroimaging, has moved from a qualitative assessment of brain structures to a much more quantitative, multimodal assessment. As radiologists, we still look to see, for example, if a brain tumor is changing in size, but we have a lot of new tools, especially MR and positron emission tomography (PET) imaging techniques, to look at physiology like blood flow, vessel permeability and metabolic changes within the tumor. We can also use MR techniques to examine the tissue for specific metabolites to develop a more accurate diagnosis and prognosis.
NewYork-Presbyterian/Weill Cornell Medical Center has been an early adopter of hybrid PET-MR imaging, with several scanners that can obtain PET and MR images simultaneously in the same machine with software that fuses the structural and functional images together. It’s so much better for our patients in terms of saving time and improving compliance, and we’re able to view different aspects of a lesion, which means better diagnoses.
Accessibility is important, too. We’re pioneering the use of a lightweight, portable MRI in our ICU, but eventually, this technology could also increase MRI accessibility in the community. With new AI techniques, the goal is to improve image quality, even with low-field magnets, while reducing claustrophobia during the procedure.
Dr. Amir Goldan and I are building a portable, high-resolution brain PET scanner to detect the earliest stages of Alzheimer’s disease. The goal is early detection, so we can offer treatments to slow the progression of the disease. Getting access to a PET scanner can be very challenging, though crucial in treating neurodegenerative disease. Our portable brain PET scanners can be attached to existing CT scanners or eventually be placed in mobile units, so people, especially in underserved communities, can access high-resolution PET imaging.
Dr. Anna Nordvig and I have been looking at how imaging can be used to assess treatment response on the new anti-amyloid therapies for Alzheimer’s. By examining early cerebral blood flow changes, we hope to predict cognitive outcomes, rather than having to wait a year or more to see whether these therapies are benefiting the patient. In the future, we hope to use these and other novel imaging techniques to monitor healthy aging in people and screen for underlying Alzheimer’s pathology, before the onset of clinical symptoms.
Summer 2025 Front to Back
-
From the Dean

Message from the Dean
In times of uncertainty, the well-being of our patients remains our true north. -
Features

Good Medicine
New research aims to extend the power of existing vaccines — and develop even better ones in the future. -
Features

Labor of Love
Weill Cornell Medicine faculty seek to better integrate family and paid caregivers into the practice of medicine, guided by the knowledge that what’s good for the caregiver is good for the patient. -
Features
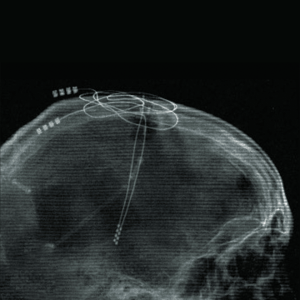
Rewired
Through deep brain stimulation and brain-computer interfaces, neurologist Dr. Nicholas Schiff (M.D. ’92) is pioneering efforts to improve life for patients with traumatic brain injury.
-
Notable

New Student Residence Completed
The new Feil Family and Weill Family Residence Hall offers a thriving environment for aspiring doctors, scientists, and health-care leaders. -
Notable

$50 Million Gift for Weill Cancer Hub East
At the Weill Cancer Hub East, experts from four leading research institutions will collaborate on research to understand the relationships between metabolism, nutrition, and cancer. -
Notable
Dateline
Dr. Radhika Sundararajan has developed an intervention to work with traditional healers to address HIV in Uganda. -
Notable
Overheard
Weill Cornell Medicine faculty members are leading the conversation about important health issues across the country and around the world. -
Notable
News Briefs
Notable faculty appointments, honors, awards and more — from around campus and beyond. -
Grand Rounds

Physician Assistants to the Fore
Aspiring medical practitioners are flocking to Weill Cornell Medicine’s physician assistant program, helping to head off provider shortages and enhance patient care. -
Grand Rounds
Biomedical Entrepreneurial Thinking
The latest cohort of the Accelerating BioVenture Innovation program makes its pitches. -
Grand Rounds
News Briefs
The latest on teaching, learning and patient-centered care. -
Discovery

Benfotiamine Boosts
Decades of work leads to clinical trial for early Alzheimer’s treatment. -
Discovery

Reducing Risk of Opioid Addiction While Alleviating Pain
A new study suggests that increasing the levels of naturally produced endocannabinoids may thwart the highly addictive nature of opioids while maintaining the drugs’ ability to relieve pain. -
Discovery

Findings
The latest advances in faculty research, published in the world’s leading journals. -
Alumni

Profiles
From supporting critically ill children and their families to negotiating licensing deals for the world's first COVID-19 vaccine, our alumni are making an impact.
-
Alumni

Notes
What’s new with you?
Keep your classmates up to date on all your latest achievements with an Alumni Note.
-
Alumni
In Memoriam
Marking the passing of our faculty and alumni. -
Alumni

Moments
Marking celebratory events in the lives of our students and alumni, including Match Day and Commencement. -
Second Opinion
Image Making
How will today’s advances in radiology transform patient care? -
Exchange

Community Outreach
A physician and a nurse discuss how engagement can transform community health and clinical practice. -
Muse

‘Settled’ by Nature
Dr. Nicole Goulet is a trauma and critical care surgeon who finds inspiration from being a lifelong athlete and outdoor enthusiast. -
Spotlight

Going Mobile
Dr. Robert Frawley (Ph.D. ’16) brings science to students aboard the BioBus.