Rewired
Features
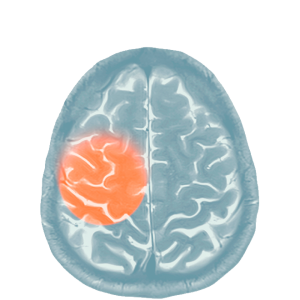
Neurologist Dr. Nicholas Schiff (M.D. ’92) has pioneered the use of deep brain stimulation in people with traumatic brain injury, helping them regain lost cognitive and motor skills. In parallel, he has worked to identify impaired patients with hidden cognitive function and is now seeking to test brain-computer interfaces that might help them.

Brain implants pulse hope
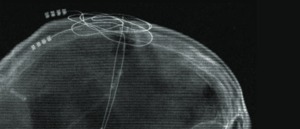
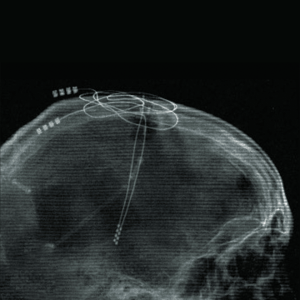
There is a lump in Gina Arata’s chest just below her collarbone. But it’s not the kind to worry about. Inside that lump is a battery and a small computer chip. A wire tunnels under the skin to the back of Arata’s neck and from there to the top of her skull, where it plunges deep into her brain. At the end of the wire, a pair of small electrodes pulse electricity into two kidney-shaped areas near her brain stem. 1
The wire is a lifeline to Arata. Twenty-five years ago, as a college senior, Arata’s car skidded and hit a telephone pole. When she awoke from a coma 14 days later, doctors told her that she was lucky to be alive. Arata had severe trauma that severed circuits in her brain, sure as her car severed that telephone pole.
Arata’s life was never the same. She finished her degree but had to forego law school and move home. She had difficulty concentrating and holding a job. There were mood swings and physical challenges. In social settings, she had trouble reading people. Then, in 2018, Arata’s father was searching the internet for treatments when he came across a call for patients to join a new clinical study. That search brought Arata to Dr. Nicholas Schiff, M.D. ’92, a neurologist and neuroscientist at the Feil Family Brain and Mind Research Institute at Weill Cornell Medicine.
Clinical precision
Dr. Schiff and his collaborator, Dr. Jaimie Henderson, a neurosurgeon at Stanford Medical Center, were looking for patients to test an experimental treatment for cognitive disabilities related to moderate to severe traumatic brain injuries. Arata became Patient 1 in a groundbreaking study. 2 “She was our astronaut,” Dr. Schiff says.
Dr. Henderson surgically implanted electrodes in Arata’s brain and those of five others (though one later dropped out due to an infection), laying claim to a region of their brains known as the central lateral nucleus, part of the thalamus.
The thalamus is, in part, a sort of relay station for four of the body’s five senses — sight, sound, touch and taste. Like a telephone operator, the thalamus handles incoming sensory information and routes it to the cerebral cortex for interpretation. 3 The central lateral nucleus, however, is unique in that it is responsible for regulating frontal areas of the brain needed for cognition. It unites sensory and motor regions of the brain with “thinking” areas of the brain.
“Deep brain stimulation in the central thalamus expands the capacity of the frontal areas of the brain to retain and work with information,” Dr. Schiff explains. “We’re restoring this cognitive processing.”
When these connections are broken, the ability to make logical, physical and emotional sense of the world is broken, too. And Arata’s brain was badly broken. Today, however, six years after implantation, her deep brain stimulator is going strong. Arata says she “feels smart again.”4 She can read and comprehend books, has a better memory, is less irritable, has fewer obsessive-compulsive tics, and enjoys greater muscle control and dexterity.
“It is both brain and motor function that have improved,” she says. “I used to fall down the stairs all the time. And I haven't done it since. When it's off, I can't spread my toes on my left foot. If it's on, I can spread them. It's the weirdest thing ever.”
For Arata’s mother, Marla, a psychologist with a clinical appreciation for all that is going on in her daughter’s brain, the transformation has been astounding. “I’ve had to raise my daughter three times — once as a child, once after the accident, and once again after the implant,” she says. “But the difference between Gina before and after the surgery has been remarkable.”
I think, therefore I am
For Dr. Schiff, the trial was a culmination of years of work on deep brain stimulation, but it was also a return to core interests in the nature of human consciousness and a launchpad toward future work potentially restoring function to patients in minimally conscious states whose awareness and communication abilities are poorer than those in the DBS trial.
His fascination with consciousness had begun as an undergraduate doing historical research at the Montreal Neurological Institute on pioneering neurosurgeon Dr. Wilder Penfield.
“Consciousness wasn’t a popular thing to study,” he recalls, seeing medicine as the best way to pursue the future of this early work.
Dr. Schiff likens the stimulator to a pacemaker for the brain. He explains that deep brain stimulation overrides the underactivated thalamic cells and activates the cells receiving the impulses, restoring the range of their function and — possibly, he stresses — rewiring new pathways. 5 Most importantly, Dr. Schiff has shown that the changes are not temporary. 6
His work is centralized around what he calls the mesocircuit hypothesis of brain injury and recovery that explains how brain circuits are damaged and how they change in response to stimulation. 7 Traumatic brain injury often widely damages the circuits of the brain, and for survivors of this type of damage, there is little hope. But results like Gina Arata’s show that if impaired cells can be kept alive, they can regain substantial function.
‘Still in there’
In 2024, Dr. Schiff and colleagues published what may be their most attention-grabbing study yet. They used fMRI and other brain imaging tools to show that a quarter of the more than 240 unresponsive patients in the study could hear and carry out complex mental tasks following spoken commands, such as “imagine yourself swimming.” The tasks required sustained effort lasting many minutes. One in four patients in the study showed brain activity in the exact regions of the brain over time as healthy people asked the same questions.
“These people, who are thought to be unresponsive, were capable of high-level cognitive tasks,” Dr. Schiff says. That means maybe 100,000 patients in the U.S. are “still in there.”
“The finding was a game-changer,” Dr. Schiff says.
In clinical terms, Dr. Schiff explains that the patients are experiencing cognitive motor dissociation — a disruption between thinking and physical movement. He is now looking to understand what causes these disruptions and, most importantly, whether once identified such persons might regain communication through brain-computer interfaces, like those that have allowed at least one patient with ALS to speak again and those with paralysis to type emails by thought alone.
“One can envision situations in which severely injured patients in minimally conscious state or who have cognitive motor dissociation might receive an effective treatment combination of deep brain stimulation and brain-computer interfaces,” he says.
While Dr. Schiff’s work on deep brain stimulation and on the nuances of cognitive motor dissociation is for now proceeding along parallel paths, he can also foresee a day when those paths converge, and similar deep brain stimulation technologies arise that might help patients recover from coma, stroke and other disorders of consciousness.
Dr. Schiff and colleagues are now focusing on bringing the central thalamic brain stimulation approach that helped Gina Arata through the regulatory process toward an FDA-approved therapy. “If we’re successful,” he says, “a therapy like this could help many people across the world with debilitating traumatic brain injury.”
- Thalamic deep brain stimulation in traumatic brain injury: a phase 1, randomized feasibility study ↩︎
- Subject and Family Perspectives from the Central Thalamic Deep Brain Stimulation for Traumatic Brain Injury Study: Part I ↩︎
- Cleveland Clinic; Thalamus ↩︎
- Subject and Family Perspectives from the Central Thalamic Deep Brain Stimulation for Traumatic Brain Injury Study: Part I ↩︎
- Local changes in network structure contribute to late communication recovery after severe brain injury ↩︎
- Local changes in network structure contribute to late communication recovery after severe brain injury ↩︎
- Recovery of consciousness after brain injury: a mesocircuit hypothesis ↩︎
Summer 2025 Front to Back
-
From the Dean

Message from the Dean
In times of uncertainty, the well-being of our patients remains our true north. -
Features

Good Medicine
New research aims to extend the power of existing vaccines — and develop even better ones in the future. -
Features

Labor of Love
Weill Cornell Medicine faculty seek to better integrate family and paid caregivers into the practice of medicine, guided by the knowledge that what’s good for the caregiver is good for the patient. -
Features
Rewired
Through deep brain stimulation and brain-computer interfaces, neurologist Dr. Nicholas Schiff (M.D. ’92) is pioneering efforts to improve life for patients with traumatic brain injury.
-
Notable

New Student Residence Completed
The new Feil Family and Weill Family Residence Hall offers a thriving environment for aspiring doctors, scientists, and health-care leaders. -
Notable

$50 Million Gift for Weill Cancer Hub East
At the Weill Cancer Hub East, experts from four leading research institutions will collaborate on research to understand the relationships between metabolism, nutrition, and cancer. -
Notable
Dateline
Dr. Radhika Sundararajan has developed an intervention to work with traditional healers to address HIV in Uganda. -
Notable
Overheard
Weill Cornell Medicine faculty members are leading the conversation about important health issues across the country and around the world. -
Notable
News Briefs
Notable faculty appointments, honors, awards and more — from around campus and beyond. -
Grand Rounds

Physician Assistants to the Fore
Aspiring medical practitioners are flocking to Weill Cornell Medicine’s physician assistant program, helping to head off provider shortages and enhance patient care. -
Grand Rounds
Biomedical Entrepreneurial Thinking
The latest cohort of the Accelerating BioVenture Innovation program makes its pitches. -
Grand Rounds
News Briefs
The latest on teaching, learning and patient-centered care. -
Discovery

Benfotiamine Boosts
Decades of work leads to clinical trial for early Alzheimer’s treatment. -
Discovery

Reducing Risk of Opioid Addiction While Alleviating Pain
A new study suggests that increasing the levels of naturally produced endocannabinoids may thwart the highly addictive nature of opioids while maintaining the drugs’ ability to relieve pain. -
Discovery

Findings
The latest advances in faculty research, published in the world’s leading journals. -
Alumni

Profiles
From supporting critically ill children and their families to negotiating licensing deals for the world's first COVID-19 vaccine, our alumni are making an impact.
-
Alumni

Notes
What’s new with you?
Keep your classmates up to date on all your latest achievements with an Alumni Note.
-
Alumni
In Memoriam
Marking the passing of our faculty and alumni. -
Alumni

Moments
Marking celebratory events in the lives of our students and alumni, including Match Day and Commencement. -
Second Opinion
Image Making
How will today’s advances in radiology transform patient care? -
Exchange

Community Outreach
A physician and a nurse discuss how engagement can transform community health and clinical practice. -
Muse

‘Settled’ by Nature
Dr. Nicole Goulet is a trauma and critical care surgeon who finds inspiration from being a lifelong athlete and outdoor enthusiast. -
Spotlight

Going Mobile
Dr. Robert Frawley (Ph.D. ’16) brings science to students aboard the BioBus.
