“Benfotiamine boosts blood levels of thiamine…to diminish Alzheimer’s pathology.”
Benfotiamine Boosts
Discovery
Decades of work leads to clinical trial for early Alzheimer’s treatment

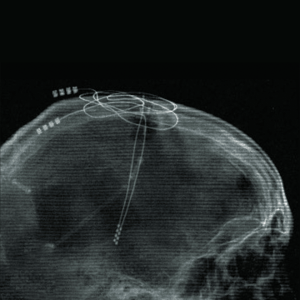
Neuroscientist Dr. Gary Gibson keeps a framed picture of a cell derived from the skin cells of a person with Alzheimer’s disease on his office wall.
The image is a memento of Dr. Gibson’s breakthrough hypothesis about an underlying cause of mild cognitive impairment and Alzheimer’s — that an insufficiency of vitamin B1 called thiamine alters the ability of mitochondria in brain cells to properly use glucose, directly causing neurodegeneration.
“It’s been well known since the 1930s that thiamine deficiency can cause dementia. However, in the late ’90s, most other dementia researchers focused instead on the discoveries of amyloid plaques and tangles of tau protein, which were posited as potential causes of Alzheimer’s. They hypothesized that these abnormal brain changes caused lower glucose metabolism,” says Dr. Gibson, a professor of neuroscience in the Feil Family Brain and Mind Research Institute. “Our approach is just the opposite: We think thiamine deficiency alters glucose metabolism in brain cells, and that’s what leads to the formation of plaques and tangles. Therefore, treating brain thiamine deficiency may be a better treatment target.”
Alzheimer’s disease affects nearly 7 million Americans, according to the Alzheimer’s Association. Yet despite its prevalence and years of research to slow patients’ decline in memory, cognition and function, there are few treatments — with only modest efficacy. Dr. Gibson’s decades of work investigating thiamine deficiency has now culminated in a nationwide clinical trial evaluating an entirely new treatment approach for slowing Alzheimer’s progression.
Early research findings support novel hypothesis
Dr. Gibson’s early basic science work at the University of California, Los Angeles, in the late 1970s found that a common form of thiamine deficiency associated with neurodegeneration in people with alcohol use disorder interferes with glucose metabolism, and that thiamine requirements varied between individuals.
That connection was an attractive stepping stone for shifting his focus to studying the underlying biology of glucose metabolism and thiamine deficiency in Alzheimer’s. In the late ’80s, he was recruited to join Weill Cornell Medicine and set up his lab at the affiliated Burke Neurological Institute. There, he and his colleagues published numerous papers on findings that supported the hypothesis that altered glucose metabolism in brain cells caused by a thiamine deficiency could be a direct cause of Alzheimer’s disease.
Starting with a compound developed in Japan in the 1960s to address vitamin deficiencies in the general population, Dr. Gibson and colleagues focused on a synthetic oral drug, benfotiamine — a precursor or “prodrug” of thiamine.
“Benfotiamine boosts blood levels of thiamine to 100 times the normal levels, enabling more thiamine to move into brain cells to restore thiamine-dependent glucose utilization processes in mitochondria, and to diminish Alzheimer’s pathology,” says Dr. Gibson, who is also a professor of neurosciences at the Burke Neurological Institute and director of the Laboratory for Mitochondrial Biology and Metabolic Dysfunction in Neurodegeneration.
In preclinical research, benfotiamine successfully addressed the clinical and biological characteristics of Alzheimer’s, including impaired cognition, amyloid plaques, abnormal accumulations of tau protein called neurofibrillary tangles, lower glucose metabolism, oxidative stress and inflammation.
“As an oral medication, benfotiamine is much more convenient, less expensive and, we believe, may do a much better job of targeting the root cause of the disease.”
First-in-human studies begin
In 2015, Dr. Gibson conducted a pilot clinical trial of benfotiamine at the Burke Rehabilitation Center to evaluate whether 12 months of treatment with the drug would enhance glucose utilization and minimize cognitive decline in patients with mild cognitive impairment or early Alzheimer’s. The study enrolled 70 patients.
The results were encouraging: Benfotiamine increased blood thiamine to high levels and showed strong signs of efficacy. For example, the increase in the Alzheimer’s Disease Assessment Scale-Cognitive Subscale, which evaluates memory, language and thinking skills in people with Alzheimer’s and other dementias, was 43% lower in the benfotiamine group than in the placebo group, suggesting less cognitive decline. Preliminary evidence from this study also showed that benfotiamine had promising potential for improving cognitive and functional outcomes.
In May 2022, the National Institute on Aging, part of the NIH, awarded the Burke Neurological Institute a $45 million grant to fund a larger clinical trial based on the strength of the trial proposal and evidence from the preclinical research and the pilot study. Dr. Gibson is working in collaboration with co-principal investigators Dr. Howard Feldman, director of the Alzheimer’s Disease Cooperative Study at the University of California, San Diego, and Dr. Jose Luchsinger, vice-chair for Clinical and Epidemiological Research at Columbia University.
The phase 2A-2B study, called BenfoTeam, will take place at 50 sites nationwide and seeks to enroll 406 patients ages 50 to 89 with mild cognitive impairment or mild dementia due to Alzheimer’s. The primary objectives are to determine the highest safe and well-tolerated dose of benfotiamine and whether it can improve global function and cognition over 18 months. The study began enrolling the first patients in April 2024, including at Weill Cornell Medicine and NewYork-Presbyterian/Weill Cornell Medical Center in September, with Dr. Anna Nordvig, the Feil Family Clinical Scholar in Neurology II, serving as site PI.
The investigators will use advanced blood biomarker technologies for their study, in collaboration with groups around the world. They will work with the University of Cambridge, U.K., to assess thiamine levels; the University of Virginia to evaluate abnormal use of glucose; the University of Gothenburg, Sweden, to assess tau tangles, neuron loss and inflammation; and C2N Diagnostics, an American company, to evaluate amyloid plaques.
“We are thrilled to have the opportunity to offer to our patients the BENFO clinical trial — the final step of a half century of research into this possible novel treatment for Alzheimer’s disease,” says Dr. Nordvig, who is also an assistant professor of neurology who collaborates with the Helen & Robert Appel Alzheimer’s Disease Research Institute, and is also an attending neurologist in NewYork-Presbyterian/Weill Cornell’s Alzheimer’s Disease & Memory Disorders Program. “I am also heartened by the preliminary results with the easy pill form showing very good drug tolerability.”
Dr. Gibson cautioned that taking over-the counter vitamin B1 supplements does not raise blood thiamine levels to the concentration required to treat the brain thiamine deficiency that occurs in AD. Thiamine prodrugs such as benfotiamine can raise blood thiamine to the levels required to treat brain thiamine deficiency. Commercially available forms are not regulated or tested for safety or efficacy. The benfotiamine in the trial is made exclusively for the trial by FDA approved methods, and participants are monitored for safety and disease progression.
“The recently approved drugs for treating Alzheimer’s, lecanemab and donanemab, are administered intravenously and work by removing amyloid plaques. They are relatively inconvenient, expensive and function to address disease symptoms,” Dr. Gibson said. “As an oral medication, benfotiamine is much more convenient, less expensive and, we believe, may do a much better job of targeting the root cause of the disease.
“The fibroblast image on my office wall represents our immense effort. It also reminds me of all the people I worked with and our rigorous experiments testing what we thought was going to be important,” he adds. “Evidence-based science takes time. It’s truly exciting to watch our lab research translate into a clinical trial testing a new treatment for a disease that affects millions of patients.”
A version of this story previously appeared in the Weill Cornell Medicine online newsroom. For more information about the trial and to locate a study site, visit ClinicalTrials.gov or benfoteam.org or call 877-807-1290 (toll-free).
Summer 2025 Front to Back
-
From the Dean

Message from the Dean
In times of uncertainty, the well-being of our patients remains our true north. -
Features

Good Medicine
New research aims to extend the power of existing vaccines — and develop even better ones in the future. -
Features

Labor of Love
Weill Cornell Medicine faculty seek to better integrate family and paid caregivers into the practice of medicine, guided by the knowledge that what’s good for the caregiver is good for the patient. -
Features
Rewired
Through deep brain stimulation and brain-computer interfaces, neurologist Dr. Nicholas Schiff (M.D. ’92) is pioneering efforts to improve life for patients with traumatic brain injury.
-
Notable

New Student Residence Completed
The new Feil Family and Weill Family Residence Hall offers a thriving environment for aspiring doctors, scientists, and health-care leaders. -
Notable

$50 Million Gift for Weill Cancer Hub East
At the Weill Cancer Hub East, experts from four leading research institutions will collaborate on research to understand the relationships between metabolism, nutrition, and cancer. -
Notable
Dateline
Dr. Radhika Sundararajan has developed an intervention to work with traditional healers to address HIV in Uganda. -
Notable
Overheard
Weill Cornell Medicine faculty members are leading the conversation about important health issues across the country and around the world. -
Notable
News Briefs
Notable faculty appointments, honors, awards and more — from around campus and beyond. -
Grand Rounds

Physician Assistants to the Fore
Aspiring medical practitioners are flocking to Weill Cornell Medicine’s physician assistant program, helping to head off provider shortages and enhance patient care. -
Grand Rounds
Biomedical Entrepreneurial Thinking
The latest cohort of the Accelerating BioVenture Innovation program makes its pitches. -
Grand Rounds
News Briefs
The latest on teaching, learning and patient-centered care. -
Discovery

Benfotiamine Boosts
Decades of work leads to clinical trial for early Alzheimer’s treatment. -
Discovery

Reducing Risk of Opioid Addiction While Alleviating Pain
A new study suggests that increasing the levels of naturally produced endocannabinoids may thwart the highly addictive nature of opioids while maintaining the drugs’ ability to relieve pain. -
Discovery

Findings
The latest advances in faculty research, published in the world’s leading journals. -
Alumni

Profiles
From supporting critically ill children and their families to negotiating licensing deals for the world's first COVID-19 vaccine, our alumni are making an impact.
-
Alumni

Notes
What’s new with you?
Keep your classmates up to date on all your latest achievements with an Alumni Note.
-
Alumni
In Memoriam
Marking the passing of our faculty and alumni. -
Alumni

Moments
Marking celebratory events in the lives of our students and alumni, including Match Day and Commencement. -
Second Opinion
Image Making
How will today’s advances in radiology transform patient care? -
Exchange

Community Outreach
A physician and a nurse discuss how engagement can transform community health and clinical practice. -
Muse

‘Settled’ by Nature
Dr. Nicole Goulet is a trauma and critical care surgeon who finds inspiration from being a lifelong athlete and outdoor enthusiast. -
Spotlight

Going Mobile
Dr. Robert Frawley (Ph.D. ’16) brings science to students aboard the BioBus.