At three weeks old, the biggest challenge for most infants is settling into a routine of feeding and sleeping. But Mila Dukes had a more frantic experience, including an exhaustive gauntlet of medical procedures. “She had a spinal tap, she had an MRI, she had a head ultrasound, a stomach ultrasound, a blood test, a vision test and a hearing test — all within a 24-hour period,” says her mother, Melanie Dukes.
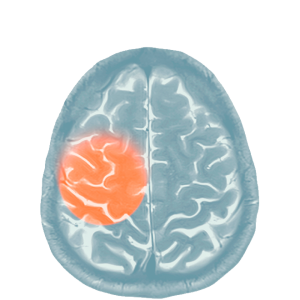
Mila was diagnosed with congenital cytomegalovirus (CMV) infection last year. CMV is commonplace, and more than half of all U.S. adults over 40 have been infected. Infections are generally asymptomatic in healthy adults, but the virus remains dormant in the body. And in pregnant people, CMV infection or reactivation of latent virus can lead to transmission to their unborn children. Congenital CMV infection affects roughly 1 in 200 newborns in the U.S., putting children at risk of hearing or vision loss, intellectual disabilities and other developmental problems.
Luckily, a statewide pilot CMV screening program in New York caught Mila’s infection early. “She is one of those babies who would’ve been completely missed because she passed the hearing screen,” says Dr. Christine Salvatore, chief of pediatric infectious disease. Dr. Salvatore subsequently took the lead on Mila’s care, overseeing the tests that ultimately led to her receiving antiviral treatment — the only pharmaceutical treatment available for congenital CMV. It was the start of a medical journey that will span Mila’s childhood, but Dukes, of Brooklyn, recognizes that her family was relatively lucky. “It gave me peace just to know that she was being checked more than any other child because of this diagnosis,” she says. But she adds that “if there had been a vaccine for pregnant women against CMV, this all could have been prevented.”
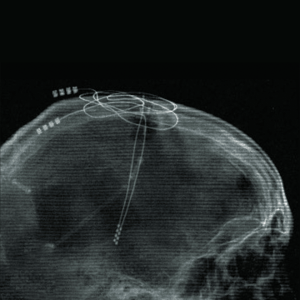
The good news is that multiple CMV vaccines are now in active development, potentially adding to the deep roster of vaccines that have saved the lives of more than 146 million children ages 5 or younger worldwide over the past 50 years and spared many more from pain and disability. “Essentially every decade, new vaccines change the face of pediatrics. This is true even now as we see new vaccines that pediatricians have wished for coming to fruition,” says Dr. Sallie Permar, chair of pediatrics, who is actively collaborating with multiple such vaccine programs.
Indeed, Weill Cornell Medicine researchers are collectively engaged in a wide range of research efforts aimed at extending the protection from existing vaccines against diseases like influenza and rotavirus. In parallel, other researchers are focused on targeting other infectious threats like CMV and human immunodeficiency virus (HIV), and better understanding the unique attributes of the immune systems in children and pregnant people that could maximize the effectiveness of vaccines. These efforts have the potential to save millions of lives worldwide and accelerate the development of even better protective measures against infectious diseases in the future — if researchers continue to receive the funding and support they need.