“The unifying thread running through my lab’s research is that bone is formed by a composite of site-specific stem cells, where each of those stem cells is adapted to meet the needs of their respective locations.”
Bones' Secret Cells
Features
Research led by Dr. Matthew Greenblatt and his lab is revealing connections between bone stem cells and a surprising array of conditions — including cancer.

For over two millennia, some cartographers have referred to unmapped regions as terra incognita, Latin for “unknown land.” Likewise, despite all that modern medical science has documented about our bodies at the microanatomical level, unknown territories — call them corpus incognito — still remain.
The urge to explore the unknown is what drives Dr. Matthew Greenblatt and his lab team at Weill Cornell Medicine. Over the last several years, they have pushed beyond the frontiers of medical science by discovering new varieties of stem cells, found exclusively in bone.
As the specialized, self-renewing cells from which all the other trillions of cells in our body ultimately derive, stem cells are critical throughout life for development, growth and healing. In this way, many diseases — as well as their potential treatments — trace back to stem cells, making their identification and characterization a high priority for medical research.
It’s little wonder that stem cells had captivated Dr. Greenblatt as a Ph.D. student initially in the field of immunology. As he realized, though, just how much the immune stem cell landscape had already been mapped out, Dr. Greenblatt instead sought to break new ground in a less-developed field.
“For me, that was bone,” says Dr. Greenblatt, an associate professor of pathology and laboratory medicine. “We want to bring bone up to that level of rigor and precision that had been the standard in immunology for years.”
The picture emerging from Dr. Greenblatt’s lab is that the building up of hard, mineralized material into sveltely precise structures that internally scaffold our bodies is far more complex than previously appreciated. His and his colleagues’ widespread investigations of uncharted bone stem cells have begun revealing connections to a surprising range of conditions — not only skeletal disorders, as would be expected, but even diseases as disparate as cancer and Alzheimer’s.
By documenting these until-now overlooked stem cells that give rise to bone making, the Weill Cornell Medicine researchers hope to blaze a trail toward new therapies for numerous, challenging diseases.
“The unifying thread running through my lab’s research is that bone is formed by a composite of site-specific stem cells, where each of those stem cells is adapted to meet the needs of their respective locations,” says Dr. Greenblatt. “And the flip side of that is, each site-specific stem cell can account for the signature disease processes of those sites.
“That new concept opens up an opportunity for us to harness the unique properties of each of the site-specific stem cells and how they act on their local environment to influence disease.”

A New Paradigm
Linked together as a skeleton, bones at first glance seem to provide little more than structural support and protection for the squishy, vital organs of our body. But in its thrift, evolution leveraged the physiological real estate that bones occupy by filling many of them with bone marrow. Residing within this spongy tissue, hematopoietic stem cells — the very first kind of stem cell ever documented, back in the 1960s — produce the various cell types found in blood.
The hidden complexity of bones extends further to how they grow. Since the 1700s, scientists have described two distinct mechanisms of bone formation: endochondral and intramembranous ossification. Most bones, including those in our limbs, ribs and spine, arise through the endochondral pathway, where rubbery tissue called cartilage forms first and then hardens into bone. Other bones, including those of the skull and our collarbones, form directly via the intramembranous route, skipping a cartilage phase altogether.
As stem cell science expanded over the past few decades, researchers managed to successfully isolate the progenitor cell that carries out that second, direct mode of bone formation — though only where new bony material forms on the inside surface, or endosteum, of bones. It had remained an open question if any distinct populations of stem cells performed the same task on the outer surface, or periosteum, of bones.
In a groundbreaking paper published in Nature in 2018, Dr. Greenblatt and colleagues answered that question in the affirmative. The Weill Cornell Medicine researchers discovered a stem cell essential for the direct growth and repair of bone’s periosteal surface. The never-before-seen stem cell came to light when the researchers added fluorescent tags to known bone formation genes. The proteinaceous product of one gene, dubbed Cathepsin K, kept appearing on bone exteriors in select cells that the researchers christened as CTSK stem cells. The researchers went on to positively identify these same sorts of periosteal bone cells in human samples.
The Nature findings, the first big result from Dr. Greenblatt’s lab, established a new paradigm that bone contains not one, but several different types of stem cells, each with unique roles and anatomic locations. The findings set the stage for the pioneering work that has followed.
“The idea that different regions of the skeleton have different stem cells, and that the outer surfaces and inside surfaces of bone are distinct, was a key takeaway from that work,” says Dr. Greenblatt. “That finding opened up so many new avenues for us to explore regarding bone stem cells and disease.”
The Outlying Spine
The waves made by that Nature paper also succeeded in attracting new talent to Dr. Greenblatt’s lab, with Dr. Jun Sun and Dr. Seoyeon Bok both coming to Weill Cornell Medicine in 2018 as postdoctoral associates in pathology and laboratory medicine. (Dr. Bok is now a research associate in pathology and laboratory medicine.) The two scientists proceeded to pursue studies into the bones comprising the spine and the skull, respectively.
“After our initial findings came out, we asked ourselves where to go next to look for new bone stem cells,” says Dr. Greenblatt, “and one of the most exciting areas to look at the time was vertebrae.”
The vertebrae constituting the spine, a set of 33 bones at birth that fuse by adulthood into around two dozen, are osteological outliers. These back bones have distinct developmental progressions and evolutionary origins from other bones, and accordingly also suffer from distinct conditions.
When Dr. Sun and colleagues examined genetic activity patterns in known skeletal stem cells at various bodily sites, a unique signature stood out for a population of vertebral cells. To verify the function of these cells, and show that they were stem cells, the researchers genetically engineered defects into them and then observed in an experimental platform that spinal bone failed to form properly.
Having validated the suspected “stemness” of the vertebral cells through this and other experiments, the researchers subsequently confirmed the cells’ presence in human spinal specimens with assistance from Dr. Sravisht “Chevy” Iyer, an assistant professor of orthopedic surgery at Weill Cornell Medicine and assistant attending orthopedic surgeon at the affiliated Hospital for Special Surgery.
As a physician who treats hundreds of patients every year with spinal maladies, from osteoporosis to generative disc disease, Dr. Iyer emphasizes the broad importance of the vertebral stem cell discovery for potentially developing new therapeutic approaches tailored to the spine’s unique biology.
“Back pain is such a common, debilitating condition and is a leading cause of missed work,” says Dr. Iyer. “Rather than interventions that assume every bone in the body is sort of the same, we expect that understanding the true biological basis of how the spine heals will allow for site-specific treatments that could be transformative.”
Keeping Spinal Cancer at Bay
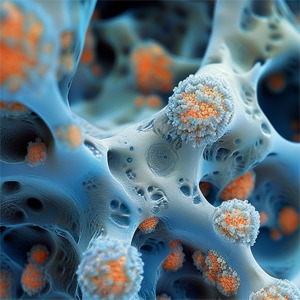
As part of their characterization of vertebral stem cells, the Weill Cornell Medicine researchers focused on one of the most perplexing spine-biased conditions: cancer metastases. Many cancers are three to five times more likely to spread to the spine than to long bones, notes Dr. Sun. That’s particularly problematic because spinal metastatic disease is notoriously difficult to treat, with patient median survival time only being 10 months.
Since the 1940s, the prevailing theory behind this metastatic mystery has been that blood flow preferentially propels tumor cells to the spine, especially when patients’ abdomens constrict during coughing or defecation, for instance. Skeptical of this eight-decade-old claim, Dr. Greenblatt and colleagues initially examined blood flow in experimental models and found no supporting evidence.
Taking a different tack, the researchers genetically engineered the newfound vertebral stem cells to lose function. Intriguingly, levels of metastasis subsequently evened out across bone types.
In another experiment, the scientists transplanted vertebral stem cells and ordinary skeletal stem cells in the leg tissue of two preclinical models, where spine bones and normal bones subsequently developed, respectively. When metastasizing cancer cells were administered to both models, the malignant cells still ended up in the spine bones grown in the leg, making clear that the disparity is not anatomical, but cellular. “Spine stem cells are more pro-metastatic than other bone stem cells,” says Dr. Greenblatt.
Next, Dr. Sun and colleagues conducted a search for any biomolecules abundantly secreted by vertebral stem cells but not by other cells. The search proved fruitful, identifying a protein called MFGE8 that acts like a magnet for many kinds of cancers.
These cumulative findings — including the vertebral stem cell discovery — took close to five years to produce. They were published in a September 2023 study in Nature, which Dr. Sun led.
Dr. Sun and colleagues are now delving into how vertebral cells regulate tumor growth after metastasis has occurred. Better understanding this could pave the way for new drugs that kill metastasized cells or, better yet, hinder their ability to take root in the spine in the first place, significantly boosting patient survival odds.
“It’s really important that we find some way to target tumor cells in the spine or prevent them from ending up there,” says Dr. Sun.

“Rather than interventions that assume every bone in the body is sort of the same, we expect that understanding the true biological basis of how the spine heals will allow for site-specific treatments that could be transformative.”
Fused Too Soon
In parallel to this spine-centered research, Dr. Bok led efforts involving the skull, exploring the idea that because skull bones grow new bone directly, any malfunctions in the newfound CTSK+ stem cells could be at the root of certain conditions. “We theorized that a large range of birth defects that kids can have in their skulls and faces could be due to this new stem cell as a shared cause,” says Dr. Greenblatt.
The researchers zeroed in on craniosynostosis, a condition that affects approximately 1 in 2,500 newborns. Ordinarily, babies’ skull bones do not fuse together in early infancy. Fibrous growth plates in the skull, or sutures, remain open to allow for brain growth. These sutures fuse normally at varying ages once rapid brain growth is complete and these growth plates are no longer needed. In craniosynostosis, however, one or more of these sutures prematurely fuse together before birth. Unless managed surgically, the condition can lead to pressure on the brain manifesting as developmental delay, impaired vision and progressive morphologic deformity.
To investigate, Dr. Bok and colleagues genetically engineered CTSK+ stem cells with a faulty gene whose loss of function had previously been shown to trigger craniosynostosis. The researchers logically expected that the altered stem cells would go into overdrive, producing too much bone and fusing skull plates. But this did not occur. Paradoxically, the CTSK+ stem cells missing the key gene instead died off at suture sites, with massive bone overgrowth still proceeding.
The Weill Cornell Medicine researchers suspected a still undiscovered bone stem cell could be to blame. Additional experiments and analyses ultimately sussed out another novel stem cell, designated as DDR2+ stem cells, whose activity is suppressed by CTSK+ stem cells. “We found that defects in the first stem cell, CTSK+ stem cells, are sensed by the second stem cell, DDR2+ stem cells, and this second stem cell attempts to compensate by undergoing maladaptive expansion,” says Dr. Greenblatt.
The surprises did not end there. As it turned out, DDR2+ stem cells produce bone differently than the two long-known means (endochondral and intramembranous), displaying endochondral ossification but without marrow formation. “This finding of ours was the first new bone formation mechanism reported in about 300 years,” says Dr. Greenblatt.
The researchers subsequently formed a collaboration with Dr. Caitlin Hoffman (M.D. ’07), a leading craniosynostosis surgeon and associate professor of neurological surgery, and Dr. Thomas Imahiyerobo, section chief of pediatric plastic and reconstructive surgery at NewYork-Presbyterian/Columbia University Irving Medical Center and an instructor in plastic surgery at Weill Cornell Medicine. With the parental consent of her infant patients, Dr. Hoffman was able to provide samples of skull tissue (which would otherwise have been discarded post-procedure) to Dr. Greenblatt’s lab. There, Dr. Bok and colleagues proceeded to identify the two stem cells of interest, CTSK+ and DDR2+ stem cells.
“It was a game changer that we could show these stem cells are true stem cells using human specimens,” says Dr. Bok, who is the lead author of a separate September 2023 study in Nature reporting the wide-ranging findings.
With an eye toward eventual therapies, the researchers isolated a growth factor protein secreted by CTSK+ stem cells that normally keeps the DDR2+ stem cells in check. Administering this protein into a research model of craniosynostosis slowed the pathological bone fusion process, pointing a way forward for skull bone targeted drugs that could limit the need for surgeries and improve patient outcomes.
“I think for sure these discoveries are going to lead to a therapeutic alteration in how we approach craniosynostosis,” says Dr. Hoffman, an associate attending neurological surgeon at NewYork-Presbyterian/Weill Cornell Medical Center. “It’s unbelievably exciting to be able to be part of a team where this kind of momentum starts being created.”
A Bone-Brain Axis?
Even though Dr. Greenblatt and colleagues have found two brand-new stem cell types functioning right inside of our own skulls, the researchers are quick to point out that the full picture of skull bone formation remains incomplete. Most glaringly, the flat bones of the skull contain marrow somehow — surprising, because the stem cells identified in the skull thus far are not known to be able to create this tissue.
In seeking to address this knowledge gap, Dr. Bok and colleagues have recently uncovered hints of a third new stem cell in the skull. Finding this candidate stem cell responsible for marrow formation could have broader implications, the preliminary work is suggesting, into a whole “bone-brain axis,” as Dr. Bok calls it, with linkages to neurodegenerative disorders.
“We’ve shown through past work and increasingly in our current work that the stem cells overlying the brain in the flat bones of the skull are uniquely adapted for bone-brain interactions,” explains Dr. Greenblatt. “These stem cells might be creating a unique environment that’s influencing brain disorders in a way that’s surprising and not previously appreciated, and also therapeutically tractable.”
In the field of neurodegeneration, inflammation has emerged as a key marker and potentially key driver of Alzheimer’s, Parkinson’s, amyotrophic lateral sclerosis (ALS) and dementia of various etiologies. Inflammation involves white blood cells and other immune system cells accumulating in certain tissues and releasing biomolecules that impact local cellular behavior.
Mounting evidence suggests that when white blood cells enter the brain, they may not come from the bloodstream directly, as has long been assumed. Instead, Dr. Greenblatt says, “white blood cells may crawl out from the flat bones of your skull,” having been produced by the local bone marrow, in turn created by specialized skull stem cells. “We’re in the process of identifying a very interesting population of new bone stem cells that could be behind this process,” says Dr. Bok.
If indeed neurodegenerative disorders of the brain could have their origins or progressions tied to the encompassing skull’s marrow, it should be possible to develop treatments that control production of localized white blood cells.
“We’re in early stages,” says Dr. Greenblatt, “but it’s something we’re deeply investigating.”
“We hope existing drugs could be harnessed to treat a surprising array of disorders that leverage these connections between local stem cells and local disease processes in the body.”
A New Emphasis on Bones
With the science of bone stem cells and related novel therapeutic approaches gathering pace, Dr. Greenblatt says that with any luck, some of the many treatments already developed for osteoporosis and other conditions will re-demonstrate their value.
“One of the bigger pictures here is that we do have drugs that target the skeleton,” he says. “We hope existing drugs could be harnessed to treat a surprising array of disorders that leverage these connections between local stem cells and local disease processes in the body.”
As he looks back on all the progress over just the past several years in delineating a whole new province in cellular biology and pathology, Dr. Greenblatt expresses optimism for future patients.
“The discoveries of these stem cells are allowing us to identify the specific biology underlying diseases that are associated with different parts of the skeleton,” Dr. Greenblatt says, crediting his fellow pioneering researchers at Weill Cornell. “Their engagement and passion have translated into tangible discoveries that we think could really make a difference.”
Summer 2024 Front to Back
-
Features
Science Over Stigma
By probing the physical cause of obesity, researchers have repudiated harmful misconceptions, leading to new, highly effective medications. -
Features

The Sounds of Science
How insights from ornithology, coupled with advances in AI, could enable doctors to screen for disease using the human voice. -
Features

Bones’ Secret Cells
Research led by Dr. Matthew Greenblatt and his lab is revealing connections between bone stem cells and a surprising array of conditions — including cancer. -
Notable

Expansion in Midtown
A 216,000 square-foot expansion of clinical and research programs at 575 Lexington Ave. will provide state-of-the-art clinical care at the Midtown Manhattan location. -
Notable

A Dramatic Growth in Research
In the decade since the Belfer Research Building’s opening, Weill Cornell Medicine’s sponsored research funding has more than doubled. -
Notable

Dateline
Heart disease presents differently in resource-poor countries like Haiti. Dr. Molly McNairy and colleagues are working to identify underlying causes and prevention. -
Notable
Overheard
Weill Cornell Medicine faculty members are leading the conversation about important health issues across the country and around the world. -
Notable

News Briefs
Notable faculty appointments, honors, awards and more — from around campus and beyond. -
Grand Rounds

Living With Endometriosis: A 12-Year Journey
How the right treatment reduced the pain of endometriosis -
Grand Rounds

Taking Action Against Lung Cancer
Monitoring by Weill Cornell Medicine’s Incidental Lung Nodule Surveillance Program can lead to early cancer detection. -
Grand Rounds

News Briefs
The latest on teaching, learning and patient-centered care. -
Discovery

Gut Check
New evidence shows that a bacterium found in the gut of livestock could be a trigger of multiple sclerosis in humans. -
Discovery
Researchers Chart the Contents of Human Bone Marrow
A new method for mapping the location and spatial features of blood-forming cells within human bone marrow provide a powerful new means to study diseases that affect it. -
Discovery

Findings
The latest advances in faculty research, published in the world’s leading journals. -
Alumni

Profiles
Forging critical connections to move research from the bench to the bedside, our alumni are making an impact. -
Alumni

Notes
What’s new with you? Keep your classmates up to date on all your latest achievements with an Alumni Note. -
Alumni
In Memoriam
Marking the passing of our faculty and alumni. -
Alumni

Moments
Marking celebratory events in the lives of our students, including the White Coat Ceremony and receptions for new students. -
Second Opinion

Equal Risk
Does race have a role in calculations of health risks? -
Exchange

Health Equity
Two faculty members discuss the importance of community-engaged research in their work to help combat cancer disparities fueled by persistent poverty. -
Muse
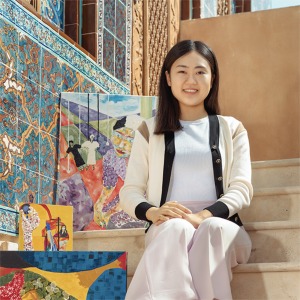
Finding Strength in Art
Surin Lee is a Weill Cornell Medicine-Qatar medical student, Class of 2026, and a visual artist. -
Spotlight

Partners in Solving Surgical Challenges
Dr. Darren Orbach (M.D. ’98, Ph.D.) and Dr. Peter Weinstock (M.D. ’98, Ph.D.) are pioneering the use of practice simulations to ensure successful complex surgeries.