“Even though it’s a huge cause of death... we know amazingly little about why people die by suicide.”
Unraveling the Riddle of Suicide Risk
Discovery
Researchers are identifying new preventive strategies by leveraging cutting-edge computational techniques and cross-disciplinary strategies.
For the past four years, much of the conversation around mental health and suicide has centered around the impacts of the COVID-19 pandemic. But U.S. suicide rates have actually been climbing for over two decades — rising by more than 35% between 2000 and 2021, according to the U.S. Centers for Disease Control and Prevention (CDC). As of 2021, suicide was the second most common cause of death among 10–24-year-olds.
Dr. Yunyu Xiao is pushing to identify strategies that could help reverse these alarming trends. She and her colleagues are leveraging a combination of cutting-edge computational techniques and cross-disciplinary insights from biology, epidemiology, economics and public health to better understand the factors that drive suicidal behavior — and the systemic disparities that put some people at greatest risk. “Even though it’s a huge cause of death... we know amazingly little about why people die by suicide,” says Dr. J. John Mann, the Paul Janssen Professor of Translational Neuroscience (in Psychiatry and in Radiology) at Columbia University and close collaborator with Dr. Xiao.
Dr. Xiao became interested in understanding health disparities while pursuing her graduate degrees in social work in Hong Kong and New York City and witnessing the vast socioeconomic divides that existed in those two major cities. As a Ph.D. student with Dr. Michael Lindsey at New York University, she co-authored an influential 2019 study that systematically analyzed demographic patterns of suicidal behavior among American high school students between 1991 and 2017.
That work revealed a notable shift away from historic patterns, according to Dr. Xiao. “Traditionally, people have always thought that it is white youths that have higher rates of suicidal ideation and attempts,” she says. But their analysis showed a striking rise in suicide attempts — the most meaningful predictor of dying by suicide in the future — and associated injuries among Black youths, and adolescent boys in particular. These findings would subsequently be incorporated into a 2019 report to Congress coordinated by Dr. Lindsey and backed by the Congressional Black Caucus, calling attention to the previously overlooked mental health crisis among America’s Black youth.
Today, Dr Xiao and her group are trying to dig even deeper, moving beyond broad categories like age, sex and race to identify more specific factors that cause certain individuals to engage in suicidal behavior. Much of this work is the product of close collaboration with experts in complementary areas of research, including Dr. Mann, a clinician specializing in causes of suicidal behavior, and Dr. Timothy Brown, associate research professor of health economics at the University of California, Berkeley.
In a study she published this past March with Drs. Mann, Brown and colleagues, the researchers obtained a vast dataset describing 306,800 suicide deaths from the CDC’s National Violent Death Reporting System. They then applied a statistical technique called latent class analysis to identify subgroups in this cohort that were experiencing shared circumstances in their lives that were meaningfully associated with suicide risk. This analysis revealed that these people could be classified into one of five groups based on life events associated with substance abuse, mental and physical health issues or relationship problems.
One of these five groups stood out in particular: the 31.7 percent of suicide deaths that were linked specifically to struggles with physical illness. Dr. Mann notes that these could represent individuals who were grappling with physical manifestations of mental health problems like depression in addition to those experiencing emotional challenges due to conditions like severe disability or chronic pain. But the people in this particular group — the largest of the five “high-risk” clusters identified in Dr. Xiao’s analysis — were generally not seeing mental health specialists prior to death and were far less likely than other groups to be taking psychotropic medications.
“This group also has the least likelihood of disclosing that they might die or attempt suicide,” says Dr. Xiao. She and her collaborators see a major opportunity to intervene by training primary care physicians to better recognize when their patients may need additional treatment for mental health conditions like depression, and emphasizes the importance of closer collaboration and communication between physicians and mental health specialists as a means for delivering more holistic care.
In the past few years, Dr. Xiao’s work has increasingly focused on an even more granular approach to assessing suicide risk based on “social determinants of health,” the confluence of diverse factors that collectively influence a person’s quality of life, such as family and social ties, the safety and amenities in their community and their education and employment status. Dr. Mann points out that these kinds of data-driven studies allow researchers to directly study how diverse, broadly representative populations are affected by their real-world environments, in contrast to other clinical studies that focus on narrowly defined cohorts of participants under carefully controlled conditions.
To effectively study these social determinants, researchers must draw on and integrate diverse data sources, ranging from electronic medical records to environmental quality data to information from sociological and economic surveys. This requires sophisticated analytical methods, and Dr. Brown and Dr. Xiao have collaborated closely to develop cutting-edge computational approaches based on machine learning and other AI techniques.
“She has developed this very sophisticated clustering algorithm that simplifies measurement of the social environment while accurately capturing the myriad of factors that make up the social environment,” says Dr. Brown, noting that this allows them to uncover hidden patterns that directly impact mental health within a given population or community. “It’s very important work, and it is super innovative. It’s the next step in learning how to measure social determinants of health.”
In one recently published demonstration of this approach, Dr. Xiao and colleagues, including Dr. Brown and Dr. Mann, used machine learning to analyze the collective impact of 84 different factors associated with social determinants of health on the physical, mental and cognitive well-being of more than 10,500 children living across the United States. Their initial analysis revealed notable patterns in terms of the impact of living conditions on children. For example, factors like high-crime environments and higher population density were generally associated with poor cognitive performance and physical health.
“This work is pretty foundational,” says Dr. Brown, pointing out that it validates the idea of using diverse data sources to identify clusters of children who are at especially heightened risk of facing additional challenges later in life while also highlighting potentially causative factors. While this initial study explored suicidal behavior as one of many outcomes, Dr. Xiao recently received funding from the National Institute of Mental Health and American Foundation for Suicide Prevention to support in-depth analyses of suicidal behavior in the future.
One critical advantage of Dr. Xiao’s social determinants-based approach: It makes it possible to implement suicide prevention measures at a larger scale while still personalizing them to some extent, enabling policymakers to make the most of every public health dollar spent. “It’s about how resources are limited... should we invest in poverty alleviation versus job availability, or should we invest in terms of education or urban planning?” says Dr. Xiao. “Our algorithm actually can calculate and inform that.”
In April 2023, Dr. Xiao was selected as a Google Research Scholar to support the further development of machine learning-based computational tools that can help policymakers weigh trade-offs and make appropriate, evidence-based decisions when designing and implementing new public health measures.
Dr. Xiao believes that broadening the conversation around suicide — by bringing to the table experts from outside the mental health world — is fundamental to her lab’s mission.
Dr. Xiao believes that broadening the conversation around suicide — by bringing to the table experts from outside the mental health world — is fundamental to her lab’s mission. In parallel, she hopes her team’s work will also catch the attention of the broader public and stimulate conversations about challenging issues that people have historically avoided discussing.
“There is a lot of stigma attached to mental health and suicide prevention,” she says. “The use of these community-based interventions can also improve people’s public awareness of social and mental health, and why certain groups of people are consistently more vulnerable.”
If you are in crisis, please call, text or chat with the Suicide and Crisis Lifeline at 988, or contact the Crisis Text Line by texting HOME to 741741.
Fall 2024 Front to Back
-
From the Dean

Message from the Dean
By integrating innovations in artificial intelligence into clinical practice, the aim is to enhance, rather than replace, the personal care that patients value. -
Features

Change of Heart
To tackle long-standing sex disparities in outcomes for cardiac surgery, Weill Cornell Medicine physicians are pursuing innovative clinical trials and treatment -
Features

The Dark Side of STING
Painstaking research has yielded vital new insights on how a protein known for triggering inflammation can both hinder — and accelerate — cancer -
Features

Teaching Empathy in the Digital Age
Meet C.A.R.L., a lifelike virtual “patient” who stands at the vanguard of advances in immersive learning that could improve the way doctors are trained. -
Notable

New Chair and Physician-in-Chief
Dr. Myles Wolf, who specializes in nephrology, will oversee Weill Cornell Medicine's largest clinical and academic department. -
Notable

Dateline
Dr. Sasha Fahme is leading studies to better understand the sexual health challenges refugee women face. -
Notable

Overheard
Weill Cornell Medicine faculty members are leading the conversation about important health issues across the country and around the world. -
Notable

News Briefs
Notable faculty appointments, honors, awards and more — from around campus and beyond. -
Grand Rounds

Lending an Ear
How a single-sided cochlear implant is helping a psychiatry resident achieve his dreams. -
Grand Rounds

The Art of Medicine
Through visits to the Guggenheim and more, medical students are expanding their thinking to improve patient-centered care. -
Grand Rounds

News Briefs
The latest on teaching, learning and patient-centered care. -
Discovery

Unraveling the Riddle of Suicide Risk
Researchers are identifying new preventive strategies by leveraging cutting-edge computational techniques and cross-disciplinary strategies. -
Discovery

A Common Type of Fiber May Trigger Bowel Inflammation
An unexpected finding could pave the way for therapeutic diets that ease symptoms and promote gut health. -
Discovery

Findings
The latest advances in faculty research, published in the world’s leading journals. -
Alumni

Profiles
From leading the Alumni Association to improving public communication of science, our alumni are making an impact. -
Alumni

Notes
What’s new with you?
Keep your classmates up to date on all your latest achievements with an Alumni Note. -
Alumni
In Memoriam
Marking the passing of our faculty and alumni.
-
Alumni

Moments
Marking celebratory events in the lives of our students and alumni, including the White Coat Ceremony and Reunion. -
Second Opinion
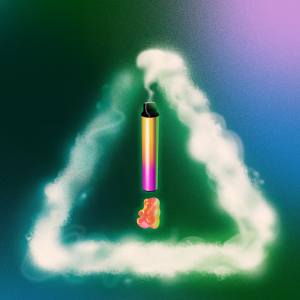
Taming Weed
How can medicine and public health address largely unregulated, readily available and potentially harmful marijuana products? -
Exchange

Roles in Research
A physician-scientist and a college student discuss how undergraduate research opportunities can boost the STEM pipeline of those from historically underrepresented communities. -
Muse

Making the Music
Clinical psychologist Dr. Robert Allan finds inspiration from composing and playing the piano. -
Spotlight

Therapeutic Advocate
In his quest to help more patients, Dr. Joseph Amprey (M.D. ‘04, Ph.D. ‘02) shifted from clinical practice to drug development.