Clockwise from left: Finding new ways to characterize and treat depression is a collaborative effort between Dr. Conor Liston (M.D. ’08, Ph.D.), Dr. Charles Lynch and Dr. Puja Parekh.

New Frame of Mind
Features
Brain science is poised to upend the way mental health disorders are diagnosed and treated — and psychiatrist Dr. Conor Liston (M.D. ’08, Ph.D.) and his team are at the forefront of this paradigm shift.

Even as a medical student, Dr. Conor Liston (M.D. ’08, Ph.D.) had questions about the way we think about and treat depression.
“I was puzzled by what is really a fundamental problem — the disconnect between our system for diagnosing depression and other mood disorders and the neurobiological basis of those illnesses,” says Dr. Liston, now associate professor of psychiatry in the Department of Psychiatry, associate professor of neuroscience in the Feil Family Brain and Mind Research Institute at Weill Cornell Medicine, and a practicing psychiatrist at NewYork-Presbyterian/Weill Cornell Medical Center.
While advances in personalized medicine, with therapeutics targeted to individual patients, are transforming the treatment of everything from cancer to heart disease, the field of psychiatry has lagged, Dr. Liston says. Yet he is convinced that neuroscience is poised to upend the way psychiatric patients are diagnosed and treated, and his Weill Cornell Medicine lab is at the forefront of that paradigm shift, part of a strategic emphasis on brain science at the institution.
At the moment, the old paradigm reigns. Despite broad consensus that mental illness is a biological disorder, specific illnesses are still diagnosed based on clusters of subjectively reported symptoms enumerated in the DSM or Diagnostic and Statistical Manual of Mental Disorders, which since 1952 has been the profession’s diagnostic bible.
“If you look at major depressive disorder, some of the nine symptoms in the DSM are even opposites,” Dr. Liston says. “Sleeplessness or sleeping all day, significant weight loss or weight gain. Patients are diagnosed with major depression if they have at least five of those symptoms, and just doing the math gives you at least 256 unique combinations. I think everyone would agree that the underlying biology of someone presenting with symptoms of agitation and sleeplessness is not the same as the patient who can barely find the energy to move.”
Even more frustrating, he says, is that first-line treatment is the same for everyone — doctors typically start by prescribing one of the selective serotonin reuptake inhibitors, or SSRIs, first introduced in the 1980s. And it’s a trial-and-error process. If after six weeks your first SSRI doesn’t work, time to try another. While existing medications and psychotherapy interventions have had transformative benefits for millions of patients, they simply do not work as well for others.
“The DSM has done a lot of good things,” says Dr. Liston. “It gave us a common language for communicating about mental illness and helped improve access to care. But there is a lot of heterogeneity among patients, and we hope that by getting at their individual neurobiology, we will be able to more immediately and effectively treat, and even come up with new ways to treat, everyone with major depression — which is a leading cause of disability and suicide risk worldwide.”

Research technician Jolin Chou
Predictive Patterns
Dr. Liston and his team’s impact reflects Weill Cornell Medicine’s commitment to understanding the brain and enhancing mental health care — one that is benefiting from emerging capabilities in imaging techniques and data science. It’s a moment when investments in these technologies and others, ranging from microscopy to artificial intelligence and genomics, are widening opportunities for practitioners of brain science that could make substantive differences for patients.
“The field of psychiatry is at an inflection point,” says Dr. Francis S. Lee, chair and psychiatrist-in-chief of the Department of Psychiatry and professor of molecular biology in psychiatry at Weill Cornell Medicine. “The groundbreaking work from Conor and his team are probably the best examples in our field of how the parallel advances in neuroscience and technology have led to categorically new opportunities to significantly improve diagnosis and treatment of psychiatric disorders.”
In a promising first step, Dr. Liston’s lab has identified different biological subtypes of depression. They’ve done this by using sophisticated computing techniques to analyze more than 1,000 resting-state functional MRIs (rsfMRIs) collected from his neuroscience colleagues across the country. Unlike standard MRIs that take pictures of the structure of your brain — to check for a tumor, for instance — this technology can observe patterns of neuronal activity by measuring oxygenated blood flow (exploiting the fact that working neurons use more oxygen).
Dr. Liston’s lab has found that these patterns of activity, also described as brain circuits, are different in people with depression than in people who are not depressed. And in analyzing those 1,000-plus rsfMRIs, and double-checking their analyses in multiple ways, Dr. Liston and his team found — and reported in a study published in Nature Medicine in 2016 — that the abnormal brain circuits of people with depression fall into four distinct patterns or subtypes. Dr. Liston believes that with even more data, more subtypes will emerge.
Can subtypes of depression be used to predict who might respond to a particular treatment? Dr. Liston believes they have that potential, and his lab has launched a series of clinical trials this year to test that hypothesis.
Analyzing data from researchers who’d been treating depressed patients with a technique known as TMS, or transcranial magnetic stimulation, his team found they could predict how patients from each of the four subtypes they’d identified were likely to respond to the treatment. A gentle, non-invasive procedure conducted in a doctor’s office, TMS is the application of a magnetic field, using a small wand with a coil at the end, to a specific area of the brain to stimulate nerve cells. It works about half the time for people with treatment-resistant depression, meaning they’ve tried one or more drugs without success. And though the U.S. Food and Drug Administration approved it in 2008, it is not yet considered a first-line treatment for depression and is usually covered by insurance only after medication has failed, a process that can take many months.
In their analysis of the TMS data, Dr. Liston’s team found that one subtype responded very well to the treatment, one moderately well, the other two not at all. This year his lab launched a multi-year study funded by the National Institute of Mental Health to test two biomarkers they’ve developed, based on those subtypes, that they believe can predict not only which patients will respond to TMS, and how strongly they will respond on a scale of 1 to 100, but more specifically how they will respond to TMS applied to two different promising parts of the prefrontal cortex.
Dr. Liston’s team expects to treat at least 350 study participants in his lab at Weill Cornell Medicine over the next five years. “Some patients improve dramatically the first time they’re treated, and that’s really rewarding,” he says. “But because it’s a double-blind study, we won’t know how well our biomarkers are actually performing to predict those outcomes until the study is completed.”
The lab is also exploring the use of a very intensive, accelerated TMS protocol to treat patients with anhedonic depression, a type of depression in which people no longer find pleasure in life and lose interest in things they once enjoyed. The three-year study, a collaboration with scientists at Stanford and UC San Diego — and with Dr. Benjamin Zebley, director of Weill Cornell Medicine’s Interventional Psychiatry Program — is funded by Wellcome Leap, a Los Angeles nonprofit whose vision for the project is “to double the number of people who receive an effective treatment [for depression] on the first try.”
“We’re trying to identify subtypes of depression within the anhedonic depression subtype,” Dr. Liston says. “A lot of people get dramatically better very quickly in response to this protocol, so we’re trying to understand which people are likely to get better so quickly, and then follow them to figure out how long the benefits last, and why some people get better and stay better and other people don’t.”
His lab is running a similar clinical trial, in collaboration with Stanford, on OCD.

‘De-Noising’ the Data
Behind this quest to rethink the way we diagnose and treat those disorders is a lab of some 30 or 40 researchers at Weill Cornell Medicine, running at least two dozen studies at any one time, to better understand what Dr. Liston describes as “the most enigmatic organ in the human body.”
Some, like Dr. Charles J. Lynch, who came to the lab as a postdoctoral fellow and is now an instructor in neuroscience at Weill Cornell Medicine, work on the human imaging side. Dr. Lynch has been doing what Dr. Liston describes as extremely important work on “de-noising” rsfMRIs — coming up with strategies to identify and either account for or completely eliminate the extraneous and potentially misleading data this tool is notorious for producing.
That complicated “de-noising” process — and the “noise” can be the result of anything from a subject’s slight head movement to idiosyncratic patterns of breathing and respiration — could help produce rsfMRIs that more reliably map an individual’s brain circuitry.
Dr. Lynch is working, not only on mapping the individual brain in more reliably granular detail, but on using that detail to further tailor TMS treatments. “In addition to the two stimulation targets Conor is testing in his current clinical trial, we are looking at potentially thousands of tiny adjustments where we might apply TMS to accommodate the idiosyncrasies of each individual’s brain circuitry and get better outcomes,” he says.
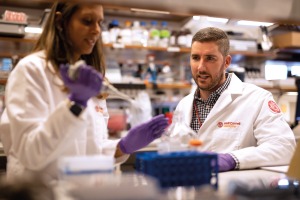
“There’s crosstalk” between investigators in the Liston lab, says Dr. Puja Parekh (left), seen here with Dr. Charles Lynch.
Other researchers, like senior postdoc Dr. Puja Parekh, are using cutting-edge tools to observe and manipulate individual brain cells in preclinical models to better understand the biological processes that underlie mood disorders.
“Conor’s group is truly unique,” says Dr. Lynch. “It’s very rare to have one lab where the expertise and the tools we use are so diverse. We’re thinking about the brain at very different levels of organization in a way that, when it works well, is very complementary.
“It’s also very rare to have a primary investigator overseeing and mentoring both neuroscience research in preclinical models and human neuroimaging research,” Dr Lynch adds. “Typically you have expertise in one or the other, but Conor is able to do both. He’s brilliant, he’s fun to collaborate with, and for all the success he’s had in such a short time, he’s incredibly humble.”
Dr. Liston has been unraveling the mysteries of neurons and brain circuits since he was an undergraduate at Harvard, where he graduated summa cum laude in 2002 and immediately published a first-authored paper in Nature on memory development in children. He has since published at least 80 more papers — on topics ranging from very specific impacts of stress and antidepressants on nerve cells to how gut microbes affect brain health. The latter, published in 2019 in Nature, was the product of an ongoing collaboration with Weill Cornell Medicine colleague Dr. David Artis, director of the Jill Roberts Institute for Research in Inflammatory Bowel Disease, director of the Weill Cornell Medicine Friedman Center for Nutrition & Inflammation, and the Michael Kors Professor of Immunology.
“Conor and I are extremely fortunate,” Dr. Artis said in a recent interview. “We happen to have met each other somewhat by chance a number of years ago, and developed a shared interest in employing broad technologies from diverse scientific fields that would normally not speak to each other to address fundamental questions in the context of gut-brain interactions that had previously been technically very challenging.”
Dr. Liston says collaboration “is central to everything we do. It’s just more fun, and it’s critical to moving the field forward. Some of the biggest problems in neuroscience and psychiatry require multidisciplinary approaches. I’m lucky to have a pretty big lab with very smart people. But no one lab can possibly have all the expertise required to really make an impact. We have a lot of collaborators, including here at Weill Cornell Medicine and at The Rockefeller University,” where Dr. Liston earned his PhD in neuroscience in 2007 as part of the institutions’ Tri-I M.D.-Ph.D. program, which also includes Memorial Sloan Kettering.

The Power of Crosstalk
If collaboration and working across disciplines is essential to the field’s progress, a cascade of elegant new technologies has been a game changer. “We can do experiments we could never have imagined doing,” Dr. Liston says. One set of techniques known as optogenetics allows neuroscientists to visualize the activity of individual neurons and turn them off and on with light. For the first time, researchers are able to not only correlate the activity of brain cells with behavior, but to tease out cause and effect.
The other big development, he says, are genetically coded calcium sensors. In optogenetics, neuroscientists figured out how to extract light-sensitive proteins called opsins from algae and insert them into the genetic code for brain cells in preclinical models. With this more recent technique, scientists insert calcium-sensing proteins into brain cells, which need calcium to become active.
“When the brain cell becomes active, calcium kind of pours into the cell and these sensors bind to it and they fluoresce, emitting green light,” Dr. Liston explains. “You can actually see it with a microscope. Each time the cell becomes active, it glows, and you get these beautiful images that kind of look like Van Gogh’s ‘Starry Night.’ So it’s the same idea as optogenetics, but instead of using light to control the activity of brain cells you’re using light as a reporter of their activity.”
Dr. Parekh came to the Liston lab in 2017 to learn those techniques and to pursue her interest in the complex interplay between stress and behavior and neural activity in the living brain. “It’s a new frontier,” she says. “The way they allow us to conceptualize the complexity of circuits and functions is pretty exciting.”
And while Dr. Liston encourages his mentees to pursue their own ideas, Dr. Parekh sees a unifying principle behind the work done in the Liston lab. “There’s crosstalk,” she says. “While the human neuroimaging side is working on improving the delivery of TMS, for instance, people in the wet lab are trying to understand how and why TMS works, which is still up in the air.”
Dr. Liston says the underlying principle of his work is one he shares with most of his colleagues in neuroscience. “The dream is not only that our efforts will transform our understanding of how the brain works, how it supports interesting behaviors,” he says, “but that our translational work — and there are people doing important work all over the country — will change the way we practice psychiatry.”
Fall 2022 Front to Back
-
From the Dean

A Message from the Dean
As an academic medical center, our tripartite mission is what drives us forward: we thrive on providing world-class care to our patients, making groundbreaking discoveries that are changing the future of medicine, and teaching the health care leaders of tomorrow. -
Features

The Search for a Cure
Weill Cornell Medicine scientists aim to liberate those living with HIV by subduing the virus for good. -
Features
Evasive Action
Could interrupting the evolutionary process of mutating cells hold the key to vanquishing cancer? Researchers led by Dr. Dan Landau are on the case. -
Features

New Frame of Mind
Psychiatrist and neuroscientist Dr. Conor Liston (M.D. ’08, Ph.D.) and his team are poised to upend the way mental health disorders are diagnosed and treated. -
Notable

New Cancer Director
Internationally acclaimed medical oncologist Dr. Jedd Wolchok, whose innovations in immunotherapy revolutionized melanoma treatment, was recently recruited as the Meyer Director of the Sandra and Edward Meyer Cancer Center at Weill Cornell Medicine. -
Notable
3 Questions
Dr. Jay Varma, director of the new Center for Pandemic Prevention and Response, explains why an interdisciplinary approach is critical. -
Notable

Overheard
Weill Cornell Medicine faculty members are leading the conversation about important health issues across the country and around the world. -
Notable

Notable News Briefs
Faculty appointments, honors, awards and more — from around campus and beyond. -
Notable
Dateline
In the global scientific effort to understand vaccine and natural immunity to SARS-CoV-2, Weill Cornell Medicine’s location in Qatar, a country of only a few million people, has been making an outsized contribution. -
Grand Rounds

Chiari Malformation
When is Surgery Necessary? -
Grand Rounds

3 Questions
Dr. Susan Loeb-Zeitlin, who worked with a multidisciplinary team to launch the new Women’s Midlife Program, shares insights about making menopause manageable. -
Grand Rounds

Social Impediments to Health
The murder of George Floyd and the resulting national reckoning on race, along with the disproportionate impact of COVID-19 on communities of color, galvanized creation of the Anti-Racism Curriculum Committee at Weill Cornell Medicine. -
Grand Rounds

Grand Rounds News Briefs
The latest on teaching, learning and patient-centered care. -
Discovery

COVID-19 and Diabetes
Basic science and clinical investigations converge to offer answers. -
Discovery

Development of Schizophrenia
Multiple changes in brain cells during the first month of embryonic development may contribute to schizophrenia later in life. -
Discovery

Findings
The latest advances in faculty research, published in the world’s leading journals. -
Alumni

Profiles
From taking the lead in newborn medicine to forging critical connections to move research from the bench to the bedside, our alumni are making an impact. -
Alumni

Notes
What’s new with you?
Keep your classmates up to date on all your latest achievements with an Alumni Note. -
Alumni
In Memoriam
Marking the passing of our faculty and alumni. -
Alumni

Moments
Marking celebratory events in the lives of our students, including Match Day, the White Coat Ceremony and Graduation. -
Second Opinion

A New Lens
What’s one way that medical education must change to better address health inequities? -
Exchange

Pivot Points
Two women leaders at Weill Cornell Medicine whose professional paths have connected discuss the power of mentorship — for themselves and other women in academic medicine. -
Muse

Two Forms of Truth
Dr. Laura Kolbe, whose poetry has garnered notable honors, talks candidly about how her writing helps her build a bridge to her work as a clinician. -
Spotlight

Building Connections
Dr. Kathleen Foley (M.D. ’69) has been bringing people together throughout her expansive career as a specialist in pain management and palliative care for cancer patients.