Just as species evolve through natural selection, individual cancer cells find ways to adapt to treatment and then evade it through an evolutionary process, notes Dr. Dan Landau, associate professor of medicine and a member of the Meyer Cancer Center at Weill Cornell Medicine, whose team is at the vanguard of this new frontier of cancer research. Their strategy: By identifying how individual cells evolve to mutate and proliferate, the scientists aim to develop tools to interrupt the evolutionary process — work key to detecting and treating cancer and avoiding unnecessary treatment.
Evasive Action
Features
Could interrupting the evolutionary process of mutating cells hold the key to vanquishing cancer? Researchers led by Dr. Dan Landau are on the case.
Data visualization: Matt Twombly
We are all born with 30 trillion or so cells that evolve throughout our lives. Even when we are healthy, these cells accrue mutations in their DNA that can then grow into “clones” or clusters of genetically distinct cells, Dr. Landau explains. “What is it that allows that single mutated cell, that is not yet cancer, to outcompete and outgrow its neighbors?” he asks. Since malignancy represents a “runaway process of evolution,” he says, it’s crucial to understand the behavior of that single misbehaving cell as an early harbinger of the malignancy process.
Dr. Landau and colleagues at Weill Cornell Medicine and the New York Genome Center are doing just that, using a set of advanced new techniques — called single-cell multi-omics — that allow them to profile thousands of individual cells in unprecedented detail.
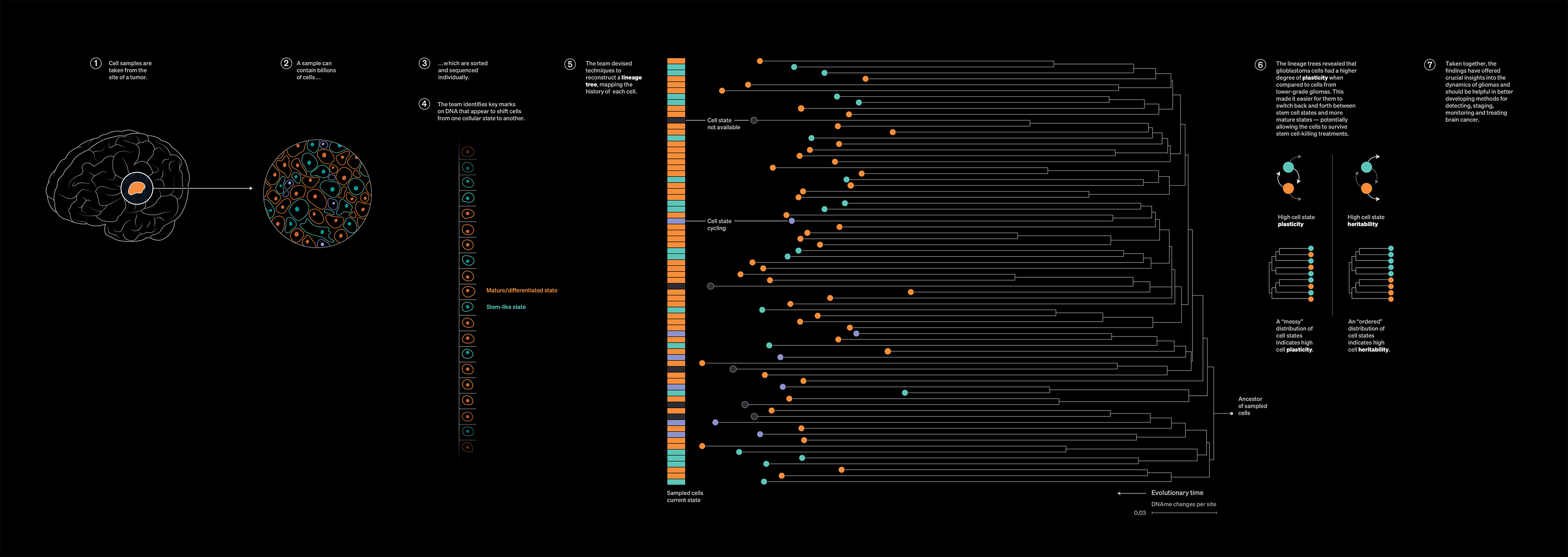
In recent work reported in Nature Genetics, the scientists sampled individual cells from patients with glioma brain tumors. In addition to mapping distinct cell behaviors in gliomas, and identifying key programming marks on DNA (called “methylations”) that appear to shift glioma cells from one cellular behavior to another, the team devised techniques to reconstruct an “ancestral tree” for each cell.
“It’s like having a time machine,” says Dr. Landau. “We can take a sample from a patient’s tumor and infer many details of how that tumor has been developing” — going back to the very origin of the tumor.
The lineage trees revealed that glioblastoma cells had a higher degree of plasticity when compared to cells from lower-grade gliomas, Dr. Landau notes. This made it easier for them to switch back and forth between stem cell states and more mature states — potentially allowing the cells to survive stem cell-killing treatments.
Taken together, the findings have offered crucial new insights into the dynamics of gliomas — information that should be helpful, Dr. Landau says, in developing better methods for detecting, staging, monitoring and treating brain cancer. And in principle, he says, “This approach could be used to study the development of many types of cancer.”
Transformative Technology
As a patient’s cancer cells evolve, clinicians need a way to detect and monitor those changes in order to better optimize treatment. In the case of many tumors, “the chance of recurrence after initial treatment is quite high, but up to now we haven’t always had a good way to detect these recurrences early, when they are most treatable,” says Dr. Landau.
That’s because existing methods for detecting DNA fragments from tumor cells — known as “liquid biopsy” because they are detected through a blood test — target a handful of specific genes or “hotspots” in the genome where cancer-associated mutations are expected. This “targeted sequencing” approach only works when DNA in blood samples includes sufficient fragments containing targeted mutations. But often following cancer surgery, the tumor burden is much too low to be detected through standard targeted-sequencing techniques.
So Dr. Landau and his team have turned to “whole genome sequencing” — allowing them to sequence all of the circulating DNA in a patient’s blood sample, which boosts the effective sensitivity by orders of magnitude. “We are able to scan the entire genome for the tens of thousands of mutations that are found in human cancer,” he explains.
In work reported in Nature Medicine, Dr. Landau and his collaborators demonstrated the value of this whole genome DNA-sequencing strategy, powered by machine learning, with blood tests on patients who had melanomas, colorectal cancers, and lung cancers. The team showed their method could detect tumor DNA in some lung cancer and colorectal cancer patients following surgery when the tumor burden is very low. “And in patients with metastatic melanoma who were being treated with immunotherapy, we could track their responses in real time,” he says.
“When we first started pursuing this strategy in 2016, everyone thought we were crazy because whole genome sequencing was prohibitively expensive,” recalls Dr. Landau. “But we developed our approach anticipating that the technology would advance and costs would come down dramatically — and they have,” he says. To speed clinical application of the new liquid biopsy platform, Dr. Landau has co-founded and is a member of the scientific advisory board of a company, C2i Genomics (see Biography).
Next Steps
Whole genome DNA sequencing, supported by machine learning, represents a “tectonic shift” in cancer research and treatment, Dr. Landau believes. Currently, without knowing whether residual cancer remains after surgery or other treatment, the paradigm is often to prescribe aggressive follow-up treatment that can carry significant side effects — and in most cases isn’t needed. And for some patients with residual cancer, the cells can adapt to treatment and evolve to become more aggressive — without doctors knowing.
“Imagine instead if you could have a simple blood test after surgery and find out yes, you do have residual disease and we can begin treatment and follow up to make sure it is working, or no, you are clear and don’t need aggressive treatment,” says Dr. Landau. His team will continue to develop their technique to be even more sensitive and specific and aim to confirm its effectiveness through clinical trials.
Fall 2022 Front to Back
-
From the Dean

A Message from the Dean
As an academic medical center, our tripartite mission is what drives us forward: we thrive on providing world-class care to our patients, making groundbreaking discoveries that are changing the future of medicine, and teaching the health care leaders of tomorrow. -
Features

The Search for a Cure
Weill Cornell Medicine scientists aim to liberate those living with HIV by subduing the virus for good. -
Features
Evasive Action
Could interrupting the evolutionary process of mutating cells hold the key to vanquishing cancer? Researchers led by Dr. Dan Landau are on the case. -
Features

New Frame of Mind
Psychiatrist and neuroscientist Dr. Conor Liston (M.D. ’08, Ph.D.) and his team are poised to upend the way mental health disorders are diagnosed and treated. -
Notable

New Cancer Director
Internationally acclaimed medical oncologist Dr. Jedd Wolchok, whose innovations in immunotherapy revolutionized melanoma treatment, was recently recruited as the Meyer Director of the Sandra and Edward Meyer Cancer Center at Weill Cornell Medicine. -
Notable
3 Questions
Dr. Jay Varma, director of the new Center for Pandemic Prevention and Response, explains why an interdisciplinary approach is critical. -
Notable

Overheard
Weill Cornell Medicine faculty members are leading the conversation about important health issues across the country and around the world. -
Notable

Notable News Briefs
Faculty appointments, honors, awards and more — from around campus and beyond. -
Notable
Dateline
In the global scientific effort to understand vaccine and natural immunity to SARS-CoV-2, Weill Cornell Medicine’s location in Qatar, a country of only a few million people, has been making an outsized contribution. -
Grand Rounds

Chiari Malformation
When is Surgery Necessary? -
Grand Rounds

3 Questions
Dr. Susan Loeb-Zeitlin, who worked with a multidisciplinary team to launch the new Women’s Midlife Program, shares insights about making menopause manageable. -
Grand Rounds

Social Impediments to Health
The murder of George Floyd and the resulting national reckoning on race, along with the disproportionate impact of COVID-19 on communities of color, galvanized creation of the Anti-Racism Curriculum Committee at Weill Cornell Medicine. -
Grand Rounds

Grand Rounds News Briefs
The latest on teaching, learning and patient-centered care. -
Discovery

COVID-19 and Diabetes
Basic science and clinical investigations converge to offer answers. -
Discovery

Development of Schizophrenia
Multiple changes in brain cells during the first month of embryonic development may contribute to schizophrenia later in life. -
Discovery

Findings
The latest advances in faculty research, published in the world’s leading journals. -
Alumni

Profiles
From taking the lead in newborn medicine to forging critical connections to move research from the bench to the bedside, our alumni are making an impact. -
Alumni

Notes
What’s new with you?
Keep your classmates up to date on all your latest achievements with an Alumni Note. -
Alumni
In Memoriam
Marking the passing of our faculty and alumni. -
Alumni

Moments
Marking celebratory events in the lives of our students, including Match Day, the White Coat Ceremony and Graduation. -
Second Opinion

A New Lens
What’s one way that medical education must change to better address health inequities? -
Exchange

Pivot Points
Two women leaders at Weill Cornell Medicine whose professional paths have connected discuss the power of mentorship — for themselves and other women in academic medicine. -
Muse

Two Forms of Truth
Dr. Laura Kolbe, whose poetry has garnered notable honors, talks candidly about how her writing helps her build a bridge to her work as a clinician. -
Spotlight

Building Connections
Dr. Kathleen Foley (M.D. ’69) has been bringing people together throughout her expansive career as a specialist in pain management and palliative care for cancer patients.